Shortly after giving birth to her son in August 2017, 27-year-old activist and Black Lives Matter icon Erica Garner suffered her first heart attack. Garner, who entered the public eye in 2014 after a police officer choked her father to death, had an enlarged heart.1 The stress of pregnancy—and perhaps the strain of her father’s death2—further weakened it. Four months later, she suffered another heart attack. This one put her into a coma from which she never awoke. On December 30, 2017, she died.3
Although all deaths are tragic, Erica Garner’s death illuminates a devastating problem in the United States: African American mothers are dying at three to four times the rate of non-Hispanic white mothers,4 and infants born to African American mothers are dying at twice the rate as infants born to non-Hispanic white mothers.5 These two trends hold true across education levels and socioeconomic status.6 Even tennis star Serena Williams—a wealthy and remarkably powerful woman—nearly died from pregnancy-related complications.7
African American women of all backgrounds—including Garner and Williams—share experiences of racial and gender discrimination. A growing body of research suggests that stress induced by this discrimination plays a significant role in maternal and infant mortality.8 This issue brief synthesizes research explaining the racial disparities in maternal and infant mortality rates and articulates how institutional racism contributes to both. It reviews empirical literature on maternal and infant mortality, concluding that the greater prevalence of maternal health risk factors among African American women cannot account entirely for their higher mortality rates. Instead, the impacts of institutional racism and sexism compromise women’s health across time, leading to poorer outcomes for African American women and infants.9 A fractured and unequal health care system and gaps in health workforce training further aggravate these racial disparities. It is racism, not race itself, that threatens the lives of African American women and infants.
Trends in maternal and infant mortality in the United States
Protecting the health of mothers and infants is a critical measure of a country’s development. By most accounts, however, the United States holds the worst records for maternal and infant mortality in the developed world. (see text box) Women in the United States are two to three times more likely to die than Canadian women in the maternal period—from the start of pregnancy to one year after delivery or termination.10 Similarly, infants in the United States have a 76 percent higher risk of death compared with infants in other wealthy nations.11 Disaggregating data by race reveals that higher rates of maternal and infant death among African American women drive the United States’ mortality crisis.
International comparisons of non-Hispanic white and African American women’s health outcomes
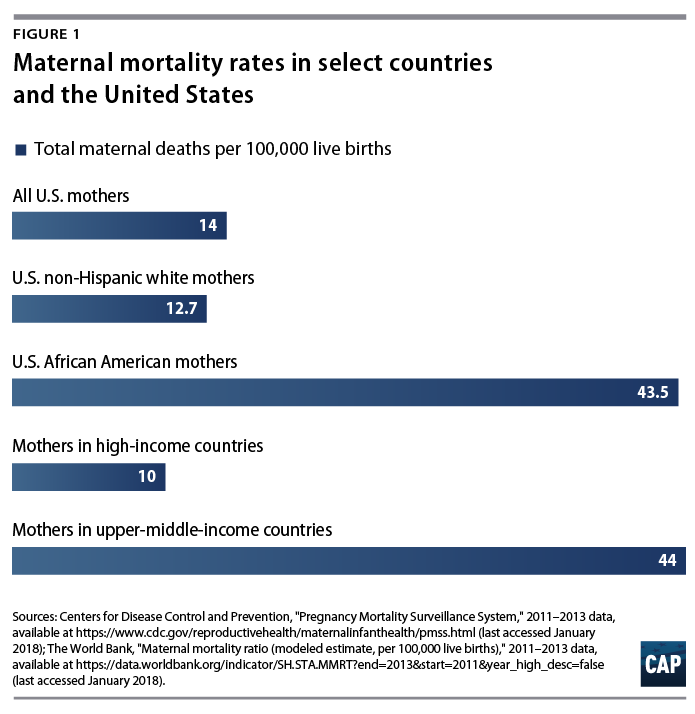
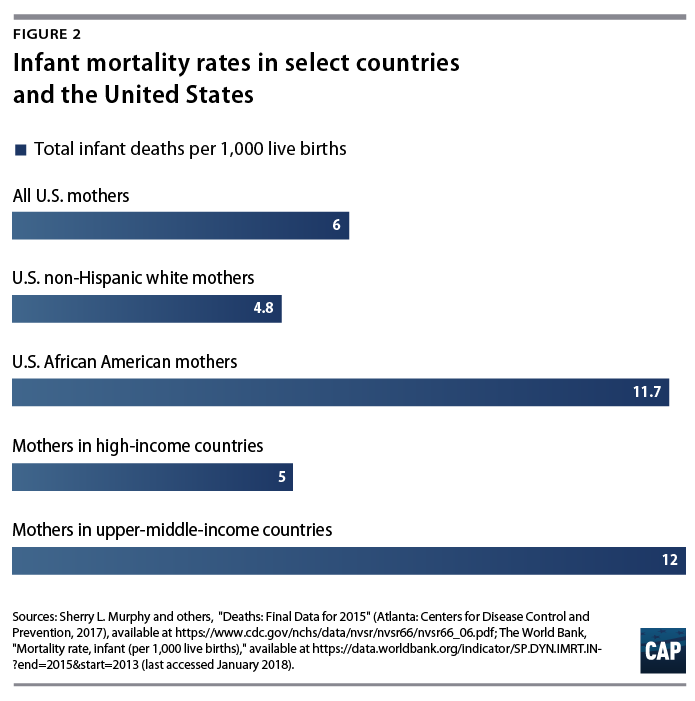
To assess maternal and infant health, public health researchers and development experts report the maternal mortality rate (MMR) and the infant mortality rate (IMR). The MMR is the number of maternal deaths per 100,000 live births annually, and the IMR is the number of infant deaths per 1,000 live births annually. Although U.S. mortality rates do not compare favorably with those of other developed countries, disaggregating data by maternal race reveals a different picture. The MMR and IMR for non-Hispanic white women in the United States are close to national MMR and IMR averages of high-income countries, whereas the MMR and IMR for African American women are closer to national averages of countries with less-developed economies.12
Maternal mortality rates in the United States plummeted over the 20th century;13 however, non-Hispanic white women experienced a steeper decline in maternal mortality than did African American women—introducing a racial gap that persists today.14 After decades of dramatic progress, maternal mortality in the United States is once again climbing for women of all races, increasing nearly 27 percent from 2000 to 2014.15 Importantly, the United States is the only developed country for which this is true.16
Like maternal mortality, infant mortality in the United States sharply declined over the 20th century. However, the racial gap in infant mortality rates has been present since these data started being collected by the government and hospitals more than 100 years ago, and it has not significantly changed in more than 50 years.17 Higher rates of preterm births and low birth weights among African American women drive this gap: African American infants are 3.2 times more likely than non-Hispanic white infants to die from complications related to low birth weight.18 Across racial groups, more deaths occur in the neonatal period—from birth to 1 month—than in the post neonatal period—from 1 month to 1 year.19
Risk factors cannot fully explain African Americans’ higher maternal and infant mortality rates
Most research on health disparities in maternal and infant mortality focus on African American women’s greater exposure to risk factors around the time of pregnancy, including poverty and low socioeconomic status; limited access to prenatal care; and poor physical and mental health.20 Although African American women are more likely than non-Hispanic white women to experience these interrelated risk factors, research shows that this greater likelihood does not fully account for the racial gap in outcomes; rather, these disparities stem from racial and gender discrimination over the life span of these women.
Poverty and low socioeconomic status
Numerous studies show that after controlling for education and socioeconomic status, African American women remain at higher risk for maternal and infant mortality. Indeed, one study showed that after controlling for income; gestational age; and maternal age and health status, the odds of dying from pregnancy or delivery complications were almost three times higher for African American women than they were for non-Hispanic white women.21 Relatedly, another analysis, controlling for the same factors, showed that college-educated African American women were almost three times more likely to lose their infants than their similarly educated non-Hispanic white peers.22
Prenatal care
Early and adequate prenatal care is designed to promote healthy pregnancies and reduce maternal and infant mortality through maternal health screening, parent education, and counseling on healthy behaviors.23 Although research shows that a lower percentage of African American women have access to prenatal care than do non-Hispanic white women, differences in prenatal care access fail to explain any racial disparities in maternal and infant mortality.24 In fact, African American women who initiated prenatal care in the first trimester still had higher rates of infant mortality than non-Hispanic white women with late or no prenatal care.25
This may partly be due to differing quality of prenatal care. Studies show that once African American women access prenatal care, it tends to be of lower quality and the women experience more complications. Current health status, health history, stress, and experiences of racism may contribute to maternal and infant mortality when coupled with lower-quality prenatal care.
Physical health
Although numerous physical health behaviors and conditions influence maternal and birth outcomes, behavioral interventions often focus on two behaviors: smoking and drug abuse and obesity. Neither of these can fully account for the racial disparity in maternal or infant mortality. Smoking and drug abuse are risk behaviors that strongly predict preterm delivery, low birth weight,26 and sudden infant death syndrome.27 However, several studies show that African American women are less likely to report smoking cigarettes than are non-Hispanic white women, and they are also no more likely to abuse alcohol or drugs during their pregnancy.28
Obesity—which is associated with pregnancy complications such as preeclampsia29—predicts both maternal and infant mortality and is more prevalent among African American women.30 Yet a recent study from the New York City Department of Health and Mental Hygiene showed that African American women of normal weight were still at higher risk of dying in the perinatal period than non-African American obese women.31 A related study comparing infant mortality rates of obese African American and non-Hispanic white mothers showed that non-Hispanic white women experienced uniformly lower risk.32 Thus, higher rates of obesity among African American women do not explain the racial disparity in infant or maternal mortality.
Mental health
When women experience acute and chronic life stressors during pregnancy, maternal mental health issues can arise.33 Yet differences in maternal mental health are also not enough to explain the gap in birth outcomes, as African American women have not consistently reported higher levels of stress during pregnancy.34 However, women of color are not typically aware of mental health symptoms experienced during pregnancy and in the postpartum period.35 This is due to a lack of knowledge regarding the signs and symptoms associated with mental health challenges. Maternal mental health issues among African American women are largely underreported and symptoms often go unaddressed.36 Moreover, mental health care is often inadequate to address the unique challenges they face as women of color, including race and gender discrimination in the workplace and beyond. These challenges have been linked to depression among this population.37
While differences in maternal mental health may not be enough to explain the gap in birth outcomes between African American women and non-Hispanic white women, they should not be ignored. In order to address trends in adverse experiences during pregnancy and the postpartum period, policymakers should consider African American women’s lack of access to appropriate mental health care screening and services as well as the link between increased stress and maternal mental health.
The cumulative effects of racism on maternal and infant health
Research that views maternal risk factors as explanations for racial disparities in maternal and infant mortality often narrowly focuses on women’s health during pregnancy. But this approach overlooks an important truth: Healthy, full-term pregnancies and safe labor are more likely to happen when women are physically and mentally healthy before becoming pregnant.
An alternative approach proposed by Michael Lu and Neal Halfon posits that racial disparities reflect altogether different developmental trajectories.38 That is, the social and economic forces of institutional racism set African American and non-Hispanic white women on distinct life tracks, with long-term consequences for their health and the health of their future children. The experience of systematic racial bias—not race itself—compromises health. African American families, for example, are offered fewer adequate housing options than non-Hispanic white families39—despite being equally qualified when comparing income levels and credit scores—and they are more likely to experience housing instability and eviction.40 During early childhood, African American girls are more likely than non-Hispanic white girls to live in substandard housing with environmental toxins such as lead that can compromise healthy development.41 Throughout school, they are more likely to be suspended or expelled than their non-Hispanic white female peers for similar behaviors.42 And once they enter the workforce, adult African American women earn only 63 cents for every dollar earned by white men,43 and they are more likely than non-Hispanic white men and women to work in jobs that lack structural supports including flexible scheduling, paid sick days, and paid family leave.44 Further, 72 percent of African American mothers are single heads of household, leading to an increased likelihood of stress.45
Taken together, these examples show that social and economic forces can profoundly affect African American women’s development across the life span. Lu and Halfon’s alternative model, known as the life course perspective, rests on two mechanisms backed by empirical evidence to acknowledge these forces: the early programming model and the cumulative pathway model.
The early programming model proposes that exposure to risk during sensitive developmental periods in early life can affect women’s health later. For example, research links maternal depression and anxiety during pregnancy to a higher risk of obesity and diabetes among offspring.46 Obesity and diabetes are well-known maternal risk factors that threaten the lives of pregnant women and their infants. In other words, the seeds of some risks are sown before a woman is even born.
In contrast to the early programming model, the cumulative pathway model focuses on stress across time, positing that chronic exposure to stress leads to allostatic load, or greater wear and tear on the body’s adaptive systems. Controlling for socioeconomic status, researchers found that African American women had the highest allostatic load scores in a sample of non-Hispanic white and African American men and women.47 This finding is also supported by other research showing that the health of African American women deteriorates more rapidly than that of non-Hispanic white women during the reproductive years.48 During pregnancy, chronically elevated levels of the stress hormone cortisol lead to immune suppression, increasing women’s risk of perinatal infections and leading to life-threatening pregnancy complications. This means that even if African American and non-Hispanic white women report similar levels of stress during their pregnancies, African American women’s increased exposure to stress throughout their lifetimes increases their allostatic load, which increases their risk of maternal and infant mortality.
Given the United States’ climate of racial inequality, African American women are more likely to experience stress during sensitive periods in early life and to be chronically exposed to stress. One would therefore expect women spared the stresses of American racial inequality during sensitive early developmental periods to have better outcomes. This seems to be the case, as black immigrant women—mostly from African and Caribbean countries—who arrived in the United States as adults enjoy better birth outcomes than native-born African American women.49 Similarly, one would also expect better birth outcomes for younger African American women, as they have spent less time exposed to the cumulative stresses of being a person of color in the United States. Indeed, studies show that African American teen mothers have lower infant mortality rates than African American mothers in their twenties.50 Since the births of young mothers are generally associated with poor health outcomes,51 this is a surprising finding and has been taken as strong evidence for the weathering52 hypothesis—the idea that cumulative stress negatively affects African American women’s health.
Social and environmental risk factors
Due to the United States’ history of racial segregation, the constellation of risk and protective factors—such as African American women having the highest rates of college enrollment out of any demographic group53—may look different for African Americans and non-Hispanic whites.54 These populations are differentially exposed to social and environmental risk factors. These risk factors55 include, but are not limited to:
- Substandard housing and housing instability
- Concentrated poverty
- Neighborhood safety
- Air quality and environmental stresses
- Poor access to quality, whole foods and adequate nutrition
- Poor access to quality, comprehensive health care services
- Unequal educational opportunities
- Poor employment opportunities, including lack of access to flexible scheduling and livable wages
- Disproportionate police violence
Problems in health care institutions may deepen racial disparities
Although evidence suggests that maternal and infant mortality are greatly influenced by mothers’ life circumstances growing up, health care institutions often deepen racial disparities. For example, women of color are less likely to have access to vital reproductive health services including family planning; abortion; and screenings for sexually transmitted infections and cervical cancer, when compared with non-Hispanic white women.56 Studies also show that African American women receive lower-quality health care generally, which results in higher risk for mortality across the life span for this population.57 This contributes to racial disparities in pregnancy-related risk factors—such as hypertension, anemia, gestational diabetes, and obesity58—and other conditions such as heart disease, HIV, AIDS, and cancer.59 Relatedly, African American infants receive lower-quality care than non-Hispanic white infants within the same neonatal intensive care units.60
Another problem is inadequate bias training among the health care workforce. In their investigation of U.S. maternal mortality, NPR and ProPublica collected more than 200 stories from African American mothers and discovered that feeling devalued and disrespected by medical providers was a unifying theme.61 Mothers also frequently reported that medical staff did not take their pain seriously, consistent with earlier studies that found pain is often undertreated in African American patients.62
Promising developments in advocacy, practice, and policy
Advocates, practitioners, and policymakers are spearheading efforts to raise awareness and address the dire state of maternal and infant mortality in the United States. For example, advocacy movements such as the Black Mamas Matter Alliance63 and the National Birth Equity Collaborative64 are creating greater public awareness through campaigns for racial and reproductive justice. A few states, including California65 and North Carolina,66 have developed health care and research collaborative groups to improve health outcomes for women and infants. Federal, state, and local leaders from various states can also share lessons learned through the Alliance for Innovation in Maternal Health and the Collaborative Improvement and Innovation Networks addressing maternal and infant health. The Health Resources and Services Administration funds these networks.67
Despite this progress, however, researchers and practitioners need better data on health disparities and a more systematic, continual review of maternal and infant deaths in order to develop prevention efforts and quality improvement programs. The following research gaps need to be addressed:
- Conduct research that substantiates the connections between a mother’s health before, during, and between pregnancies as well as that of her child across the life course.
- Conduct comprehensive, nationwide data collection on maternal deaths and complications—with data disaggregated by race, geography, and socioeconomic status.
- Produce data sets that include information on social and environmental risk factors for women and infants of color.
- Conduct better assessments and analysis on the impact of overt and covert racism on toxic stress and pregnancy-related outcomes for women and infants of color.
- Conduct research to identify best practices and effective interventions for improving the quality and safety of maternity care.
- Conduct research to identify best practices and effective interventions, as well as health outcomes before and during pregnancy, in order to address predisease pathways of adverse maternal and infant health.
- Conduct research to identify effective interventions for addressing social determinants of health disparities in maternal and infant health outcomes.
Federal policies such as the Maternal Health Accountability Act of 2017 can support state and tribal efforts to collect some of these data,68 but data collection alone is insufficient. Supporting research that aims to better understand maternal risk factors—much like the Mom’s Opportunity to Access Health, Education, Research, and Support for Postpartum Depression Act—will be important for future policy efforts.69 Furthermore, centering the lived experiences of African American women and the effects of those experiences on pregnancy-related outcomes are essential in order to fill gaps in research and develop sustainable policy and program solutions that help curb disparities in maternal and infant mortality.
Conclusion
Although recent attention on cases such as those of Erica Garner and Serena Williams shed light on an important problem, real change will require greater knowledge of why African American women and infants are most likely to die as the result of pregnancy-related complications. Greater political will is also essential to undoing the legacy of racism in the United States, which is a contributing factor in maternal and infant mortality among African Americans.
Racism’s harmful effects must be dissected to adequately address racial disparities in infant and maternal health. And once racism is taken into account, public policy and program solutions must be developed to dismantle it—spurring a lasting impact on health outcomes. The lives of African American women and infants depend on it.
Cristina Novoa is a policy analyst for Early Childhood at the Center for American Progress. Jamila Taylor is a senior fellow at the Center.