At some point in their lives, most sexually active people will be infected with a sexually transmitted infection, or STI. About 20 million new cases of STIs are diagnosed annually. Despite being a common, preventable, and treatable health problem, a lack of information, shame, and stigma tend to characterize the nation’s discussions about STIs—even though they represent a severe risk to the public and economic health of the United States.
Several U.S. populations—including women, people of color, those living in rural communities, and lesbian, gay, bisexual, and transgender, or LGBT, individuals—are especially at risk and are also less likely to have access to testing and treatment. Given the number of people affected by STIs and the billions of dollars in annual costs associated with STIs, it is imperative that policymakers continue to support a wide range of health care professionals and facilities, as well as increase and expand funding sources to meet the health needs of both patients and the public.
This issue brief begins by discussing the disparities in access to sexual and reproductive health care, including the glaring disparities in how STIs affect people of color. It then investigates how $16 billion dollars is spent annually on STI treatment and complications, as well as the personal stigma experienced by individuals diagnosed with an STI. The third section explores the types of health care facilities that provide the best care for STIs and the importance of multiple funding streams for STI testing and treatment. Lastly, the brief offers several policy recommendations—including the need to expand Medicaid, increase Title X funding, and sustain a variety of health care funding options and facilities—that would ensure that everyone who needs STI testing and treatment is able to access those services.
STI rates
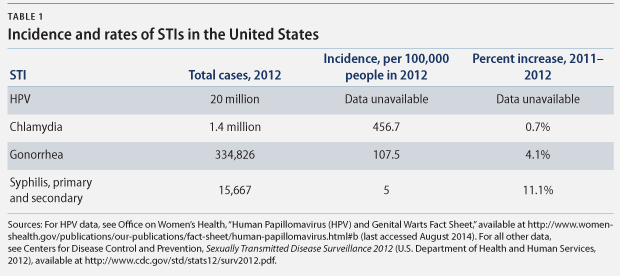
Commonly transmitted diseases such as chlamydia, gonorrhea, and syphilis are all on the rise, with increased rates of infection between 2011 and 2012. (see Table 1) The rise in gonorrhea rates is particularly concerning since the infection has progressively developed resistance to treatment. Human papillomavirus, or HPV, which can lead to health complications such as genital warts and cancer, continues to be the most common STI, accounting for the highest number of annual and existing cases. According to health officials, nearly all sexually active individuals will be infected with HPV at some point, despite the fact that there is now a vaccine that prevents it.
Disparities in STI rates and access to care
STIs disproportionately burden certain segments of the population, including some racial and ethnic groups, people living in rural and Southern regions of the United States, the LGBT community, and women.
Race
Nearly all STIs affect blacks and Hispanics at higher rates than whites. The chlamydia rate among Hispanics, for example, is more than twice the rate among whites: 380.3 cases per 100,000 people compared with 179.6 cases per 100,000 people, respectively. The gonorrhea rate among blacks—462 cases per 100,000 people—is an alarming 15 times the rate among whites—31 cased per 100,000 people. Moreover, the rate of syphilis for blacks is 6.1 times that of whites, at 16.4 cases versus 2.7 cases per 1000,000 people, respectively.
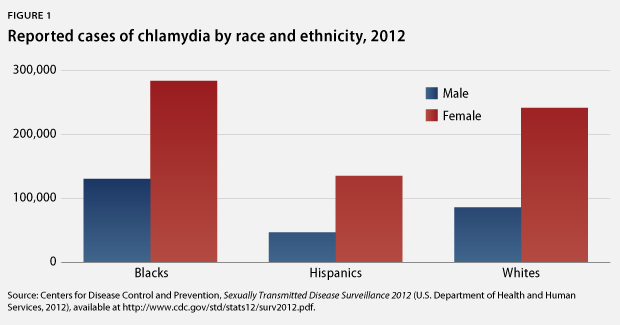
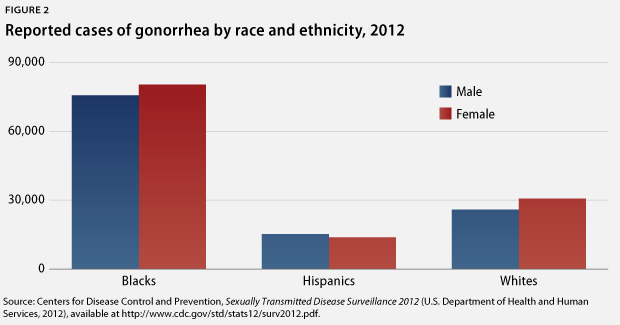
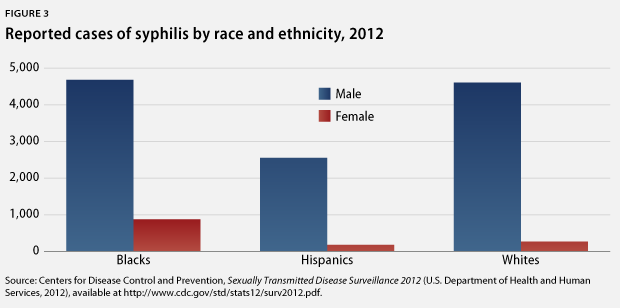
Not only are members of some racial and ethnic groups more likely to be infected with an STI, they are also less likely to receive treatment and more likely to be reinfected once they have been treated. From a behavioral perspective, it is much harder to avoid STIs when many of one’s potential sex partners—others in the community—are infected. This situation is compounded by the fact that many racial and ethnic groups also face more barriers to care—such as cost, language obstacles, lack of access to information, and logistical barriers, including limited clinic hours and a shortage of transportation options. From a structural viewpoint, such barriers are connected to poverty, low education attainment, and a mistrust of the health care system, all of which contribute to the cyclical continuation of these racial and ethnic disparities.
Region
The Southern and Midwestern regions of the United States also experience an increased prevalence of STIs. According to the Centers for Disease Control and Prevention, or CDC, the rates for chlamydia and gonorrhea are highest in the South and Midwest, while rates for syphilis are highest in the South and Northeast, suggesting similar structural barriers to health care access as those mentioned above. HPV vaccination rates in the South are also incredibly low, a trend that has caused significant concern among the reproductive health and medical communities. In comparison to the Northeast—where HPV vaccine initiation and completion rates for girls were 37 percent and 23 percent, respectively, in 2010—the initiation rate in the South was only 14 percent and the completion rate just 6 percent. In order to receive the maximum effect of the HPV vaccine, one must receive all three doses. Many young people start or initiate but do not complete the series due to financial reasons, changing providers, or family relocation.
These findings are particularly worrisome because rates of cervical cancer are also higher in the South than in other regions of the United States. If low rates of HPV vaccination in the South continue, the region could experience a strain on their resources for cervical cancer treatment. However, not all women in the South are at the same risk for developing HPV-related cervical cancer; white women are more likely than women of other races or ethnicities to initiate and complete the vaccine. This trend—likely due to some of the barriers to access discussed above—demonstrates the ways in which factors such as race and place can intersect to further restrict access to important sexual health care.
Although the same HPV vaccine initiation and completion data are not available for adolescent boys in the South, a CDC study on U.S. teens ages 13 to 17 revealed that the vaccination initiation rate for boys nationwide has increased 13.8 percent—from 20.8 percent in 2012 to 34.6 percent in 2013. However, the vaccination completion rate is much lower, increasing from 6.8 percent in 2012 to just 13.9 percent in 2013. While HPV is traditionally seen as a greater risk for women because of its association with cervical cancer, HPV also places men—especially those who have sex with men—at risk for anal and throat cancer.
LGBT
LGBT people, especially men who have sex with men and transgender women, are at greater risk for STIs. While individual behaviors such as unprotected sex play a role in increasing STI risk, so too do systemic factors. For the LGBT population, similar to other populations disproportionately affected by STIs, low socioeconomic status, discrimination at individual and institutional levels, and one’s power and position in society factor into heightened risk. LGBT people may face discrimination, ignorance, and stigma at clinics and medical offices, making it less likely that they will seek and return for treatment.
Two trends within the LGBT community are particularly alarming:
- The prevalence of HIV among transgender women: Transgender women are 49 times more likely to have HIV than other adults of reproductive age. While transgender individuals are some of the most stigmatized members of
within the LGBT community and society at large, specific individual risks often include being the receptive partner in anal sex and using unsafe needles for hormone treatments.
- The lack of research on lesbian, gay, or bisexual women: While extensive research exists about men who have sex with men and STIs, women who have sex with women are rarely mentioned in the scientific literature, perhaps due to the common misconception that STIs cannot be passed between women. However, women who have sex with women can transmit STIs during sexual contact. STIs commonly found in women who engage in same-sex contact include chlamydia, herpes, HPV, lice, and trichomonaisis. While some of these STIs are not commonly discussed, it is nonetheless important for all women to receive education about their risk level. Furthermore, providers must rely on a thorough medical history instead of labels. A woman who identifies as gay or lesbian may not only have sex with women. Similarly, a woman who currently only has sex with women may not have been gender exclusive in the past. Previous or concurrent sexual encounters with men may increase the risk of some STIs in both parties.
Gender
STIs naturally discriminate between men and women, as well as some transgender people, on the basis of anatomy. For instance, the vagina is more susceptible to infection because of its thin tissue. Furthermore, women are less likely to notice STIs, either because they are not symptomatic or because the symptoms are easily confused with normal vaginal discharge. Women may also have increased STI risk because of factors such as poverty, as well as the social norms that dictate women’s acquiescence to unsafe sex.
Women with STIs often develop more serious complications than men, some of which can severely affect their fertility. For example, 10 percent to 20 percent of women infected with chlamydia or gonorrhea develop pelvic inflammatory disease, or PID, which can lead to infertility, ectopic pregnancy, and chronic pelvic pain if they do not receive treatment. Given that more than 80 percent of chlamydial infections and up to 80 percent of gonococcal infections in women are asymptomatic, regular screening is integral to avoiding future complications. Chlamydia and gonorrhea can also cause negative pregnancy outcomes, such as neonatal ophthalmia—inflammation or infection of the newborn’s eyelid tissue—or neonatal pneumonia. Syphilis infections can be transmitted in utero, resulting in fetal death or an infant born with disabilities. Screening for and treating STIs throughout pregnancy, however, can prevent all of these outcomes.
The cost of STIs
It is easy to dismiss STI prevention and testing as too expensive. While data on the exact costs of preventive screening have not been calculated, they likely vary by region, testing site, insurance, and type of test. However, STIs and their complications amount to about $16 billion annually in direct medical costs. HIV imposes the largest financial burden, costing $12.6 billion in direct medical costs, followed by HPV at $1.7 billion, chlamydia at $156.7 million, gonorrhea at $162.1 million, and syphilis at $39.9 million.
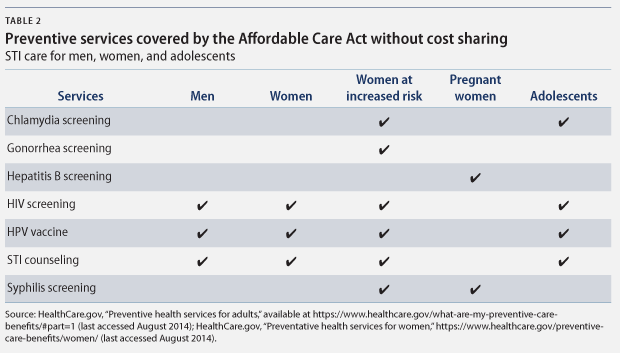
The amount that each individual pays out of pocket for STI-related health services varies based on insurance status—whether the person is uninsured, privately insured, or covered by Medicaid. Under the Affordable Care Act, many reproductive health care services are covered as preventive services and provided with no additional cost to patients. Medicaid also covers annual screening and counseling for some populations, particularly those designated as being “at increased risk.” While this policy is a step in the right direction, annual screening may not be adequate, especially for those at increased risk for STIs who are more likely to require multiple screenings throughout a given year.
What does increased risk mean?
Based on guidelines from the U.S. Preventive Services Task Force, the Centers for Medicare and Medicaid Services determines increased-risk sexual behaviors as any of the following:
- Multiple sex partners
- Using barrier protection inconsistently
- Having sex under the influence of alcohol or drugs
- Having sex in exchange for money or drugs
- Engaging in sexual activity at age 24 or younger
- Having an STI in the past year
- IV drug use (increased risk only for hepatitis B)
- Men who have sex with men
However, the lifetime cost of an STI is not universal; it is often much higher for individuals who develop complications due to an untreated STI. Unfortunately, women bear the brunt of this financial inequality since they have an increased likelihood of complications. For instance, chlamydia and gonorrhea can both result in PID, which has a host of complications noted above. Because of this, the lifetime cost per case of chlamydia can be more than $360 for women, while it is usually around $30 for men. HPV can cause cervical cancer, which can lead to an enormous increased lifetime cost. Of course, men are not immune to developing STI complications. HPV can be particularly dangerous, leading to higher rates of anal and throat cancers in men who have sex with men and people with HIV.
Stigma
For many people, STIs have more than just an economic cost, causing societal, interpersonal, and emotional costs as well. Aside from the secondary health problems that can result from having an untreated STI, the stigma associated with STIs can affect emotional health and sexual relationships. Jenelle Marie—the founder of The STD Project, a website aimed at reducing the shame associated with STIs—frequently writes about her experience living with an STI:
Diagnosed and shamed by my family doctor, I rode home with my mother in tears—convinced I would never have a ‘normal’ sex life, a loving partner, or a healthy relationship ever again. In the years that followed, I was cast out of the church and labeled a harlot, made to sleep separately from friends during overnight stays for fear of transmission, and called a bevy of names.
Stigma is not only emotionally harmful, it can also be a powerful barrier to seeking care, especially if the disapproval comes from or is perceived to come from a health care provider.
STI testing and treatment sites
The fact that STIs are easily preventable and treatable makes the increasing rates of gonorrhea, chlamydia, syphilis, and HPV especially alarming. In addition to more comprehensive education about how STIs are transmitted, policymakers must ensure that all populations, especially those at higher risk, have access to a variety of testing and treatment sites. Testing and treatment sites for STIs and HIV include the following:
- Private providers
- Health maintenance organizations, or HMOs
- Publicly funded clinics, which may or may not receive Title X funds
- Community clinics, such as federally qualified health
- Independent reproductive health clinics, such as Planned Parenthood
- Hospital outpatient clinics
- School-based clinics
- Public health clinics
- Other
- Employer or company clinics
- Inpatient treatment in hospitals
- Emergency rooms
- Urgent care facilities
Let’s look more closely at publicly funded clinics, which provide care to some of the highest-risk and most-affected populations and do a better job of screening for STIs than private providers.
Publicly funded clinics
While a majority of women who received any sexual or reproductive health service from 2006 to 2010 received the service from a private doctor, women increasingly rely on other service sites such as publicly funded clinics.
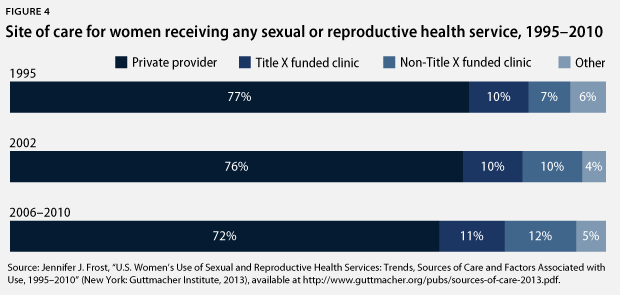
Publicly funded clinics have seen an increase in patients over the past two decades. In 1995, 17 percent of women who received any sexual or reproductive health service did so from a publicly funded clinic. That share rose to nearly 25 percent in 2006 through 2010, according to the most up-to-date available data. Furthermore, patients at publicly funded clinics are more likely to receive STI care at these facilities. From 2006 to 2010, nearly half of women who sought services at publicly funded clinics—independent reproductive health clinics, health department clinics, and community clinics—received an STI or HIV service, while only about 31 percent of women who visited a private provider or HMO for their sexual and reproductive health care received STI or HIV care.
This trend could be due to several factors. While the higher STI screening rates at a publicly funded clinics suggest that private providers lag behind on implementing current protocols or fail to inform patients of STI screening options, they also reflect the standards and regulations of care that come with Title X funding—while not all publicly funded clinics receive Title X funds, more than 4,100 do. Title X clinics, for example, must provide patients with screenings for symptomatic and asymptomatic STIs. These screenings are often performed concurrently with other reproductive and sexual health care at publicly funded clinics, meaning that they offer patients comprehensive care. All types of publicly funded clinics were more likely to provide STI care in their mix of services than private providers. Publicly funded clinic visits also involve a discussion of condoms—the only way to protect against STIs other than abstinence—more often than visits to a private provider.
Title X funded clinics serve approximately 5 million clients annually, many of whom would otherwise fall through the cracks. Title X clinics are particularly appealing to several at-risk populations, including low-income individuals, people with substance-abuse problems, people with limited English abilities, the LGBT community, and adolescents. A key reason for the appeal of Title X clinics is that many of their staff receive specific training on how to serve at-risk populations, which helps to create a more welcoming and culturally sensitive environment to which at-risk individuals are more likely to return.
Paying for STI care
In addition to reliably providing STI services, publicly funded clinics are also crucial to meeting the financial needs of patients. At Title X sites, 24 percent of patients are publicly insured, 9 percent are privately insured, and 64 percent are uninsured. In 2012, Title X clinics served more than 4.8 million clients, most of whom were female, poor, uninsured, and younger than 25 years old—in other words, populations that are at risk for STIs on multiple levels. Many patients who access Title X funded services do not meet the eligibility requirements for Medicaid, meaning that they rely on Title X funding to subsidize their care.
Those who do meet the eligibility requirements for Medicaid or Medicare can utilize coverage for STI testing, treatment, and counseling. Medicaid and Medicare cover chlamydia and gonorrhea screening for pregnant women and women who are at increased risk; syphilis screening for pregnant women and at-risk individuals, both men and women; and hepatitis B screening for pregnant women. Under certain circumstances, these plans also cover up to two individual in-person counseling sessions, which focus on STI education and prevention, annually.
Not only does public insurance provide STI care for millions of patients, its enrollees are more willing to have their insurance cover services at an STI clinic than those who were uninsured or privately insured, according to a New York City study. Because Medicaid is not employer funded and does not send explanations of benefits, or EOBs, enrollees are assured of privacy and confidentiality. For these and other reasons, including the comprehensive and preventive STI care offered through public insurance, Medicaid and the expansion of Medicaid under the Affordable Care Act are extremely important, particularly when it comes to ensuring that people continue to be tested and treated for STIs.
Similar information on private insurance coverage and STI care is lacking, most likely because privately funded STI care programs are not tracked nationally. However, the CDC has explicit guidelines for STI services, recommending annual testing for HIV, chlamydia, and gonorrhea for certain populations, as well as syphilis, HIV, chlamydia, and hepatitis B screening for pregnant women. Unlike Title X clinics, however, these recommendations do not necessarily become practices for private providers.
Policy recommendations
- Increase Title X funding: Title X funding has decreased more than $31 million dollars since 2010. Appropriating more funds to Title X would ensure that safety net programs remain in place for people who may not be insured under the Affordable Care Act or qualify for Medicaid. Title X funded clinics also offer a more comprehensive package of services than many other health care providers, ensuring their patients receive comprehensive sexual and reproductive health care.
- Expand Medicaid in all states: 23 states have not yet expanded Medicaid coverage, leaving millions of people uninsured. More than 4 million adults will fall into the coverage gap, including nearly 3 million women. In order to provide adequate care for the populations most vulnerable to STIs, all states must expand Medicaid.
- Promote education for primary care providers: Only 46 percent of women who saw a private provider for STI testing, treatment, or counseling reported that their provider discussed condom use with them. Primary care providers must remain educated about STI rates and risks, as well as incorporate questions about sexual and reproductive health care into regular visits.
- Present accurate information about STIs as part of sex education curricula: Sex education is particularly important because young people are at extremely high risk for STIs. Comprehensive sex education has been shown to reduce STI rates. Comprehensive sex education programs, with open and fact-based discussion about sex, do not encourage earlier sexual initiation or increase the number of sexual partners among sexually active teens.
- Protect patient information: Guaranteeing privacy and confidentiality is more important than ever now that young adults can stay on their parents’ health insurance plans up to age 26. The National Chlamydia Coalition cites EOBs as “a major threat to confidentiality for minors and young adults.” EOBs are currently sent to the policyholder in an effort to prevent fraud but may inadvertently notify parents that their dependents are seeking STI services. Policy changes that should be considered include determining if EOBs can be provided directly to the patient or if EOBs are necessary at all.
- Expand expedited partner therapy, or EPT: In 2006, the CDC recommended that providers who treat a patient for chlamydia or gonorrhea also provide treatment for the patient’s partner without examining the partner. As of July, 28 states and the District of Columbia allow EPT in some or all STI cases.
- Explore funding from private grants for public programs and expand the rollout of successful pilot programs: The lack of federal funding for sexual and reproductive health services means that policymakers must explore other options. The New York City Department of Health and Mental Hygiene pioneered a novel effort by partnering with the New York Community Trust—a private entity—to fund a pilot program for in-school STI testing. Because private funders are not bound by some government restrictions, they may be able to fund programs considered controversial or unorthodox.
Conclusion
Given the sheer number of individuals who seek STI care at publicly funded clinics—whether community, independent, health department, or Title X clinics—as well as the fact that the most-comprehensive STI care is provided at these clinics, it is absolutely imperative to the health of the nation that all service sites remain open and accessible even with expansion of people covered by private insurance. These sites should work in conjunction with private providers and educational services to prevent the spread of STIs and promote their treatment. Through these efforts, individuals who are affected by STIs will have the necessary access to treatment and care that they need, and the nation will begin to see progress in decreasing the rates of infection and stigma associated with STIs.
Donna Barry is the Director of the Women’s Health and Rights Program at the Center for American Progress. McKinley Sherrod was an intern with the Women’s Health and Rights Program at the Center.