At some point in their lifetimes, 99 percent of sexually active women in the United States use contraception. While this oft-cited statistic illustrates the prevalence and near universality of contraception among American women, the use of and access to family planning services varies greatly. Women access family planning in a variety of locations, as well as pay for the services they receive in a multitude of ways. Although each and every woman in that 99 percent has family planning in common, their needs are all met differently. Policy and funding decisions must recognize these differences in order to support all women in the ways that work best for them.
This issue brief discusses the importance of family planning and the benefits of making a societal investment in this much-needed health service. In addition, it highlights disparities in access to family planning services and provides information about where women receive and how they pay for services. Finally, this brief offers policy and funding solutions that will reduce disparities in access to family planning.
The importance of family planning
Family planning is important, not only because of the sheer number of women who use contraception but for economic and societal reasons as well. Women’s ability to control their fertility through preventive care in the short term has long-lasting and far-reaching consequences. Whether through reducing the cost of unintended pregnancies or enabling women to advance their education and careers, family planning provides women with greater independence to make crucial life decisions on their own terms—decisions that affect not only their lives but also the greater society.
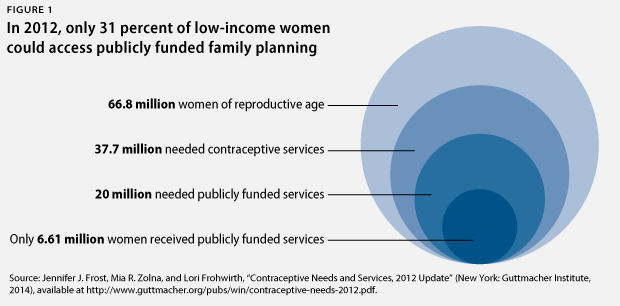
In 2012, there were 66.8 million women of reproductive age—girls and women between the ages of 13 and 44. Of that number, 37.7 million women were in need of contraceptive services, an 11 percent increase from 2000. Of these women, 20 million required publicly funded services; this was a 22 percent increase from 2000. While the number of women of reproductive age remained stable, the number of adult, low-income women increased. However, publicly funded clinics were only able to meet 31 percent of that need, a 10 percent decrease from 2001. These data demonstrate that even though women have an increasing need for family planning, fewer are actually receiving care.
In need of contraceptive services
Women who are sexually active and able to become pregnant but are not pregnant and do not want to be pregnant
The 2006–2010 National Survey of Family Growth, or NSFG, included the following services
under family planning:
- A birth control method or prescription for a method
- A checkup or medical test related to using a birth control method
- Counseling about birth control
- Counseling about sterilization
- Emergency contraception, or EC—also known as the morning-after pill—or a prescription for EC
- Counseling or information about EC
- Sterilizing operation
Results from the 2006–2010 NSFG show that almost 25 million women received contraceptive services each year, with a birth control prescription the most common service at 20.6 million women. Family planning constitutes a critical piece of our nation’s reproductive health and general health care system due to the millions of women who use these services every year.
Family planning is also important for its role in preventing unintended pregnancies. About half of all pregnancies are unintended, and the total public cost of unplanned pregnancies is estimated to fall between $11 and $12 billion annually. Yet many of these expenditures could be reduced through increased funding for family planning. The Guttmacher Institute calculates that every dollar spent in the Title X family planning program results in $7.09 in savings, which resulted in $13.6 billion in total savings in 2010. Some $5.3 billion of these savings comes from the services provided by Title X-funded clinics alone.
In 2010, Title X program data showed that the average cost for a Medicaid-covered birth was $12,770. In contrast, the per-client cost for contraception provided through Title X clinics in 2010 was $269. Private providers also experienced a similar return, spending $600 million on Medicaid-covered contraception and saving $3.5 billion in Medicaid-covered costs related to pregnancy and infant care. In both the public and private sectors, funding for family planning reduces future expenditures.
Title X and Medicaid
- The Title X Family Planning Program is, according to its website, “the only federal program dedicated to providing family planning services to individuals disadvantaged because of income or age.” In addition to funding direct services, Title X funds are used to support staff salaries, patient and public education, and community outreach. They are also used to subsidize rent, utilities, and infrastructure. In 2012, Title X “served nearly 4.8 million people, 92 percent of whom were women.”
- Medicaid, on the other hand, is a joint state-federal insurance program for eligible, enrolled, low-income individuals that directly reimburses providers. Medicaid covers a comprehensive variety of services such as preventive care, prenatal care, and long-term care, and it has become the largest source of public family planning spending, covering voluntary family planning services since 1972. In 2010, Medicaid had a total enrollment of 66.4 million people, 58 percent of whom were women.
Women and their families also benefit from family planning, which provides opportunities for both educational and career advancement. With a reduced risk of unintended pregnancy, women can more easily pursue professional occupations and increase their earning power, alleviating some of the gender wage gap. With the ability to control their fertility, women can plan and delay family leave from the workforce. This in turn allows them time to increase their work experience and wages, which will be helpful if and when they take leave in the future. When asked about the outcomes of their contraception use, women report being able to “take better care of themselves or their families, support themselves financially, complete their education, or get or keep a job.” Family planning can also improve children’s well-being, reflecting a benefit not only to parents but to children as well. Infants born less than 18 months after a biological sibling tend to have worse birth outcomes, including low birth weight and small size for gestational age, and they are more often born preterm. Moreover, parents who experience an unplanned birth are less prepared for parenthood. This affects the parent-child relationship and parents’ investment in their children. When families grow, parents’ economic and emotional investments in each child naturally decrease. Family planning allows parents to time and space each pregnancy and, subsequently, to prepare for the necessities of each child.
More concretely, access to contraception has enabled women to better time their pregnancies. Over the past four decades, as increasing numbers of women take full advantage of educational and professional opportunities, the average woman’s age at first birth has risen. Since 1990, pregnancy rates for women over age 30 have consistently increased, while rates for women under age 30 have consistently decreased. This nationwide trend has similarities at the state level. Since 2000, 46 states and the District of Columbia saw an increase in the rate of first birth for women ages 35 to 39, and 31 states and the District of Columbia experienced an increase for women 40 to 44 years old. Additionally, the teen birth rate has experienced a particularly large drop, decreasing by two-thirds since 1957. It reached a historic low in 2009, with a teen pregnancy rate of 65.3 per every 1,000 women ages 15 to 19.
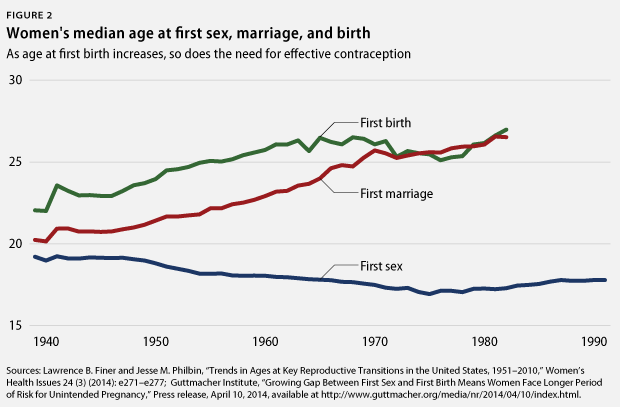
Later-first-birth rates underscore the critical importance of family planning. Women are of reproductive age and sexually active for decades and need effective contraception to plan their individual and family lives. However, not all women have the same level of access to family planning services.
Disparities in access
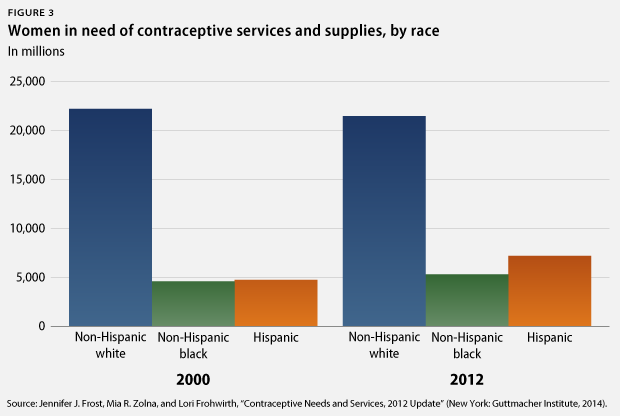
Ethnic and racial disparities are very well documented and stark with regard to family planning use and outcomes. Black and Hispanic women are less likely to use the most effective contraceptive methods than white women—58 percent and 64 percent, respectively, compared with 70 percent. The 2006–2010 National Survey of Family Growth reported the following percentages of each group that requested counseling about emergency contraception: white at 5.7 percent, black at 12 percent, and Hispanic at 18 percent. Tellingly, the percentage of unintended pregnancies for each group shows the outcomes of poor access to the most effective forms of contraception. In 2008, the percentage of unintended pregnancies for white women was 42 percent, but it rose to 56 percent for Hispanic women and to 69 percent for black women.
Barriers in access to contraception for African American and Hispanic women may be related to overall health care barriers, which include health care coverage, ongoing source of care, and quality of care. Other barriers include disparate access to health information, contraception myths, and increased apprehension of side effects. Some apprehension may stem from historical coercion to use highly effective methods, such as unnecessary hysterectomies on poor black and Puerto Rican women in teaching hospitals in the 1970s. In the early 1990s, judges in several states offered women— usually low-income women of color—the contraceptive implant Norplant to avoid jail sentencing for child abuse or drug use during pregnancy. Immigrant women face their own unique barriers to family planning services because they are, according to the authors of “Moving Forward: Family Planning in the Era of Health Reform,” “less likely than U.S.-born women to use preventive reproductive health services, including contraceptive services.” Additionally, language can be a barrier to general health care services and contraceptive knowledge and use. Fear of anti-immigration policies can also deter undocumented women from seeking health care services.
Women who live in rural areas also face barriers to accessing general health care, which in turn restricts their access to reproductive and family planning services. More than 60 million people in the United States live in a rural area, defined as a nonmetropolitan county with fewer than 35 people per square mile. In 2010, 49 percent of U.S. counties— encompassing 8.2 percent of all women—lacked an obstetrician-gynecologist. Rural populations experience unique challenges in their environment. People living in poverty in rural areas are less likely to have Medicaid or other insurance coverage than their urban counterparts. Moreover, even though almost 25 percent of the U.S. population lives in a rural area, only 10 percent of physicians practice in these regions, requiring long-distance travel for many patients. All of these obstacles interact to create a very difficult process for rural women seeking reproductive and general health care services.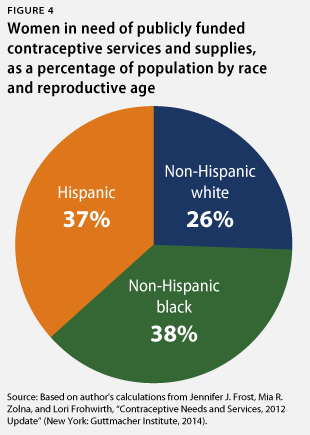
Members of the lesbian, gay, bisexual, and transgender, or LGBT, community experience exceptional obstacles to family planning. Although partially attributed to general health care barriers, this difference is also due to fear of provider bias, leading to delay in gynecological screening exams. Other challenges include stigma, violence, substandard care, and denial of care altogether. LGBT individuals report that their patient-provider relationship is often characterized by negative experiences, disrespectful treatment, harsh language, or blame for an illness on sexual orientation or gender identity. Additionally, providers’ lack of awareness of the community’s health needs, particularly the needs of LGBT women, can hinder proper care. Because many LGBT women have been sexually active with men at some point in their lives, family planning services and counseling are recommended. Contraceptive use is also important for reasons other than pregnancy prevention, such as to protect against ovarian cancer and treatment of polycystic ovary syndrome and endometriosis. Understanding the needs of LGBT women is necessary to provide appropriate care and to close gaps in coverage.
Adolescents and minors also face barriers to accessing family planning services. Although the Supreme Court ruled in 1977 that minors have a right to privacy with regard to contraception, 20 states currently only allow certain categories of minors to obtain contraceptive services without parental consent. Worries about confidentiality may discourage youth from using their parents’ private insurance as teens, and young women are less likely than women in their 30s to pay for a contraceptive visit with insurance.
Economic status and insurance coverage also influence women’s access to family planning. Women without insurance are significantly less likely to receive sexual and reproductive health services than those with public or private insurance. This year, nearly 30 percent—or 5.8 million—of the women accessing publicly funded services are not covered by any type of insurance. Addressing this need and increasing access to family planning could help reduce low-income women’s unintended pregnancy rate, which is more than five times higher than the rate for higher-income women. Furthermore, more than 6 in 10 women who receive family planning services from a publicly funded clinic also rely on this site for their general health care. For uninsured women and women with a lack of financial resources, publicly funded clinics provide services that may be inaccessible elsewhere. A diverse system of providers and locations is crucial to ensure that all women receive the services they need.
Women of all backgrounds experience disparities in access to long-acting reversible contraceptives, or LARCs, such as intrauterine devices, or IUDs, or implants. Only 8.5 percent of U.S. women use these forms of contraceptives even though they are the most effective at preventing pregnancy. In addition to the stigma against and mistrust of IUDs, the high cost of this method—which can be $500 up to $900 for women without insurance—is another reason many women choose other options. Yet improved devices, updated guidelines, and contraception coverage under the Affordable Care Act, or ACA, have contributed to the growing rate of women who choose LARCs.
Adolescents may face a provider bias against LARCs. However, the World Health Organization, the American Academy of Pediatrics, and the American Congress of Obstetricians and Gynecologists are influential organizations that have recently updated guidelines to support LARC use for young women, noting that such forms of contraception are safe and effective at any age.
Case studies
Increasing access to LARCs plays a role in reducing the number of unintended pregnancies. St. Louis, Missouri, and the state of Colorado have recently engaged in projects to provide LARCs free of cost to program participants.
- St. Louis: The Contraceptive CHOICE Project was run by researchers at Washington University in St. Louis to “promote the use of long-acting reversible methods of contraception … by removing financial and knowledge barriers” to reduce unintended pregnancies in the area. The study enrolled 9,256 women ages 14 to 45 who met a number of criteria and were, importantly, interested in starting a new contraceptive method. Participants were counseled on all reversible methods, with an emphasis on LARCs, and were provided their choice of contraception at no cost. Sixty-seven percent of participants chose LARCs, and researchers found a statistically significant reduction in abortion rates, repeat abortions, and teenage birth rates, noting a relationship between the provision of no-cost contraception, the promotion of LARC use, and a decrease in unintended pregnancies. In 2008, the rates of pregnancy, birth, and induced abortion for teens in the United States were 158.5, 94, and 41.5 per 1,000, respectively. Remarkably, the annual rates between 2008 and 2013 for females 15 to 19 years old enrolled in the CHOICE Project were 34, 19.4, and 9.7 per 1,000 pregnancies, births, and induced abortions, respectively.
- Colorado: Researchers at the University of Colorado implemented a pilot program at two health care providers to provide postpartum LARCs, specifically implants, free of cost to adolescent and young adult female patients. All adolescents and young adult females ages 13 to 24 years old attending the Colorado Adolescent Maternity Program were eligible to participate in the study. Of the eligible 396 participants, 171 patients, or 43.2 percent, chose to receive immediate postpartum implants; 86.3 percent of these patients continued use at 12 months after delivery, effectively reducing repeat pregnancies.
- Another program run through the Colorado Family Planning Initiative funded LARC provision at little or no cost through clinics in counties containing 95 percent of the state’s population. This initiative resulted in an increase in LARC use from 5 percent to 19 percent for low-income 15- to 24-year-olds from 2009 to 2011. Once again, phenomenal health improvements were seen. From 2007 to 2011, the fertility rate for 15- to 19-year-olds declined from 91 births per 1,000 women to 67 births per 1,000 women. For this age group from 2008 to 2011, the abortion rate declined 34 percent, from 11 per 1,000 women to 7 per 1,000 women.
Accessing family planning services
Women access family planning services in a variety of locations. While some information is available regarding women who access these services from private providers, most data are related to publicly provided services through places such as Planned Parenthood clinics or community health centers.
Where women receive family planning services
Results from a 2013 survey provide a breakdown of site of care for birth control among women ages 15 to 44 who had sexual intercourse and used birth control in the previous year:
- Private provider or health maintenance organization: 61 percent
- Community health center: 6 percent
- Family planning clinic or Planned Parenthood: 10 percent
- School or school-based clinic: 3 percent
- Other (includes drugstores and other unspecified sites): 17 percent
- Don’t know/refused: 2 percent
Publicly funded sites remain a necessary and important part of our health care system. Women who receive care from a publicly funded site do so in a variety of facilities:
- Independent family planning clinic: 9 percent
- Community clinics: 8 percent
- Public health departments: 6 percent
- Hospital outpatient or school-based clinics: 5 percent
These sites must be available for women who do not have access to a private provider.
Title X funding is especially important to women facing barriers in accessing care. The only federal funding source specifically for family planning, Title X supports nearly 4,200 centers that in 2010 served the vast majority of women who received services from a publicly funded clinic. The women who most frequently visit Title X clinics are in cohabiting unions, in nonmetropolitan areas, in poverty, uninsured, and are African
American or Hispanic. The challenges these women face necessitate the availability of publicly funded clinics that can serve their needs. Furthermore, clinics must be able to serve women of all backgrounds in a culturally competent manner.
Title X supports a variety of types of public clinics, including health departments; federally qualified health centers, or FQHCs; centers operated by Planned Parenthood affiliates; and centers operated by hospitals and other agencies. Health departments comprised 53 percent of Title X sites in 2010 and served 36 percent of women who received care from centers that year. FQHCs made up 14 percent of sites and served 9 percent of women, Planned Parenthood-affiliated centers made up 13 percent of sites and served 37 percent of women, and hospital- or other agency-operated centers made up 20 percent of sites and served 18 percent of women.
Emergency contraception, another key family planning option, is taken after sexual intercourse to prevent a pregnancy, and women access it differently than other forms of family planning. Of those women who obtained EC from 2006 to 2010, only 23 percent received the pills or a prescription from a private provider, while 52 percent went to a publicly funded clinic. The remaining proportion of women received care from an “other” location. This difference may be due to the high cost of EC, which can range in pharmacies from $26 to $65; stigma associated with an EC request; and/or concerns about confidentiality, especially for adolescents.
An analysis of where women access services then raises the question of how women pay for these services. Whether patients pay through private or public insurance or out of pocket, this ability can determine whether, where, and how women seek reproductive health services.
Paying for family planning
Most women are able to acquire contraception either through full or partial coverage by private insurance, and a small proportion of women use public insurance. However, data from 2013 show that nearly one in five women do not have coverage for contraception and that many of them pay out of pocket. This lack of coverage could be due to lack of insurance or to what is termed a “grandfathered” insurance plan that is not yet required to cover preventive services without cost sharing under the Affordable Care Act.
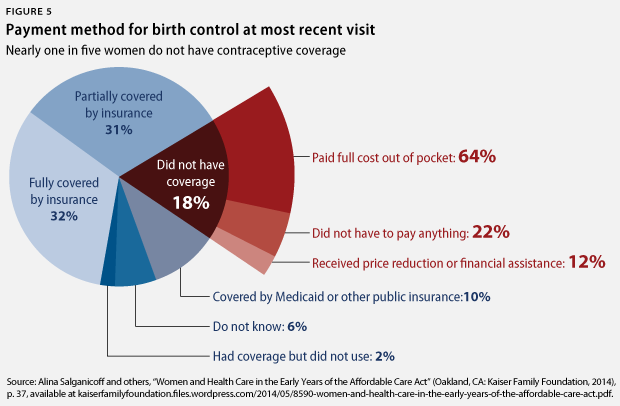
Prior to the ACA, women with private insurance often had a co-payment to cover their services and contraceptive methods. Fortunately, the ACA’s preventive care provisions have contributed to an increase in the share of women with no out-of-pocket costs for all contraceptives approved by the Food and Drug Administration, including oral contraceptives, from 14 percent in 2012 up to 56 percent in 2013. The additional 24 million co-payment-free oral contraceptive prescriptions saved privately insured women a total of $483.3 million in 2013, or an average of $269 per person.
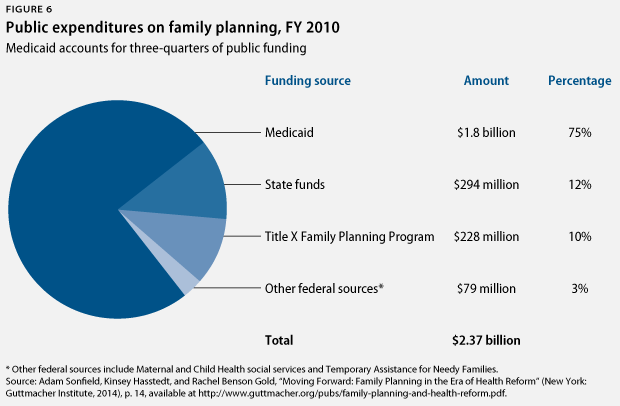
Many women do not have private insurance and must pay for services out of pocket. Between 2006 and 2010, 9 percent of women who received contraceptive services paid for their contraceptive services visit with their own income only or with another source. However, women who qualify for government assistance can use state and federal funding to pay for their family planning services as well as for their general health care needs. Medicaid accounts for the largest portion of public expenditures for family planning services. In fiscal year 2010, it accounted for $1.8 billion, or 75 percent of the nearly $2.4 billion in public spending on these services. Between 2006 and 2010, 17 percent of women who received contraceptive services paid for their health care visit with Medicaid. Medicaid is an important social safety net program that ensures women’s well-being and provides access to important family planning services.
The ACA and Medicaid expansion
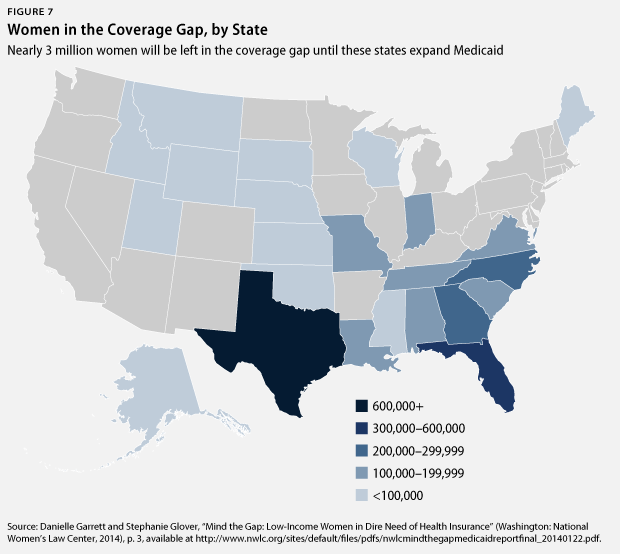
Medicaid expansion through the ACA has enabled states to increase their coverage and new patients to qualify for assistance. Before the ACA, Medicaid coverage depended on income, pregnancy or children, and disability. Following the expansion, women qualify for Medicaid solely based on income, “[marking] the first time that low-income, childless women would have access to Medicaid coverage.” Yet, as of September 2014, 23 states have chosen not to expand Medicaid, leaving nearly 3 million women in a coverage gap. As a result, these low-income, uninsured women also experience a heath care gap and are significantly less likely to access basic health care and use preventive services than other low-income, insured women. Uninsured women also experience more diagnoses of advanced-stage diseases and higher mortality rates for certain diseases than do insured women. In 2013, 58 percent of low-income, uninsured women reported that cost prevented at least one doctor’s visit within the past year, almost 150 percent more than low-income, insured women facing cost barriers. This lack of health insurance prevents low-income women from accessing the care they need, both for their reproductive health as well as for their general health.
The impact of Hobby Lobby
While the Obama administration recently introduced new rules to ensure no-cost-sharing contraceptive coverage for all women covered by private insurance, in the June 2014 decisions in Burwell v. Hobby Lobby Stores,
Inc., and Conestoga Wood Specialties Corp. v. Burwell, the Supreme Court ruled that closely held corporations can claim religious objections and exclude certain types of contraception from their employees’ insurance coverage. This decision directly affects the 23,000-plus employees of the two companies who rely on their jobs for health insurance coverage. Hobby Lobby refuses specific coverage of two types of emergency contraception and two types of intrauterine devices, while supporters of this decision suggest that women can pay for these forms of contraception out of pocket or find other coverage. However, for store employees who only earn $14 per hour if full time and $9 per hour if part time, these methods may prove to be financially out of reach. Furthermore, EC and IUDs are very expensive and therefore more difficult to obtain. Justice Ruth Bader Ginsburg even noted in her dissent that “the cost of an IUD is nearly equivalent to a month’s full-time pay for workers earning the minimum wage.”
This court decision has the potential to greatly impact low-wage workers across the country. A 2009 study found that more than half of the U.S. workforce is employed at a closely held corporation—about 75 million American workers. With 71 other companies and more than 47 pending lawsuits from for-profit companies challenging the contraception provision in court, many more women are at risk of losing their coverage. It remains to be seen if the new rules the administration suggested in August 2014 will suffice to guarantee coverage for all privately insured women.
Policy recommendations
In order to reduce disparities in access to family planning, enable more women to access services, and provide an effective and efficient method of payment for these services, we recommend taking the following steps.
Increase Title X funding
Even after implementation of the Affordable Care Act, women will still rely on Title X for a variety of reasons, including lack of insurance, services not covered under Medicaid or private insurance, and confidentiality. Title X clinics also provide reproductive health services that can be unavailable from other providers. Even though women’s dependence on publicly funded clinics has increased over the past four years, Title X has seen a decrease in funding over this same period of time. Increased funding is necessary to meet all women’s family planning needs.
Expand Medicaid in all states
The 3 million women in the coverage gap resulting from non-Medicaid-expanding states face barriers to good reproductive and general health services. This lack of insurance leads to poorer health outcomes for women who often need the care most. State expansions will enable more women to take better care of themselves and their health, as more than 7 million women stand to gain coverage if all states expand Medicaid. Increasing women’s access to health care coverage will help reduce disparities in outcomes and allow more women to lead healthier lives.
Promote the use of long-acting reversible contraceptives, especially postpartum and postabortion
Not only are LARCs more effective than other forms of reversible contraception, but they are also more cost efficient. Imperfect contraceptive adherence accounts for more than half of all medical costs associated with unintended pregnancies, and a switch from short-acting reversible contraception such as oral contraceptives to a LARC method would save $288 million per year. St. Louis, Missouri, and the state of Colorado have both recognized the importance of LARC promotion, and other cities and states should follow their lead. In addition to general LARC use, women should have the option of immediate postpartum LARC insertion—within 10 minutes of birth—which reduces the expulsion risk by 40 percent. Six states currently approve Medicaid-funded postpartum LARC insertion, and other states should follow this lead. Postabortion LARC insertion should also be available for all women, whether they have public or private insurance.
Stop state-based prohibitions to Planned Parenthood
In recent years, a number of states—including Indiana, Arizona, Kansas, North Carolina, Tennessee, and Texas—have attempted to defund Planned Parenthood through state-level legislation that would remove the organization’s public funding. Although courts have blocked most of the laws from taking effect, asserting that these laws violate an individual’s freedom to choose a health care provider and that states cannot restrict options according to the services a provider offers, Kansas and Texas successfully challenged these rulings through federal appeals courts. As a result of the appeals, Kansas has stripped Planned Parenthood of its federal funding, and Texas has stripped it of both its federal and state funding. One-third of Planned Parenthood’s budget comes from federal, state, and local government funding, and without this support the many women who rely on the organization will face obstacles in accessing needed care.
Improve sex education in schools
Although the U.S. teen pregnancy rate is at an historic low, the rate is still the highest among developed countries. Because abstinence-only sex education has proven to be ineffective and withholds important sexual health information, schools should implement a more comprehensive curriculum that is age appropriate and medically accurate. Only 22 states, including the District of Columbia, currently mandate any form of sex education, and only 13 states require that sex education, when provided, be medically accurate. Providing confidential access to family planning services via school-linked health centers has also been shown to help prevent unintended pregnancy.
Protect confidential medical information
The enactment of the ACA extended coverage to previously uninsured people as well as to dependents up to age 26, broadening the group of patients with confidentiality concerns. Privacy is a top priority among young women, and teenagers and young adults are less likely than older women to pay for contraceptive services with insurance. However, young women are also the least aware that private insurance companies send explanations of benefits to primary policyholders, frequently parents. When young women are forced to include their parents in sensitive decisions, they are more likely to avoid seeking care rather than to disclose personal medical information. Title X and Medicaid already include confidentiality protections for family planning services, but private insurance companies should expand privacy protections for both web-based and paper communication as well.
Provide cultural competency training for providers
Cultural competency refers to the convergence of behaviors, attitudes, and policies that enables effective cross-cultural work, an essential approach in reducing health disparities. Providers must have the ability to acknowledge cultural differences, understand one’s own culture, and view behavior within a cultural context. Cultural competency is important for family planning providers, who often engage with patients regarding very personal health decisions. Title X emphasizes the importance of cultural competency skills and recommends working with community partners such as school districts, social service organizations, and faith-based institutions to develop positive practices. All providers should incorporate cultural competency training in their practices to ensure more positive health outcomes for patients.
Conclusion
Family planning remains a critical aspect of ensuring women’s sexual and reproductive health as well as providing women with social and economic benefits. However, women’s unique backgrounds and experiences necessitate access and availability to family planning services with a variety of service locations and payment methods.
Improvements must be made to our current health care system so that all women can access and receive the contraceptive services they need. With the above proposals, women will have the assurance that family planning options are dependable and available. A nationwide recognition of the importance of family planning will ensure better outcomes for not only women but for their families and communities as well.
Donna Barry is the Director of the Women’s Health and Rights Program at the Center for American Progress. Amelia Esenstad was an intern with the Women’s Health and Rights Program at the Center.