“Families talk about the Head Start program with joy, and they love being in the program, so in rural communities we have to embrace that role as the compass for families. Not to intervene, but to partner with them in raising their families, to help show them the way in the face of toxic stress.”
–Missouri Head Start program director1
Introduction and summary
Nome, Alaska, situated on Alaska’s west coast near the Arctic Circle, boasts postcard-worthy views of the state’s wilderness and is the finish line for the Iditarod Trail Sled Dog Race.2 It is also home to nearly 4,000 residents and serves as the hub for nearby Kawerak Head Start, a grantee that operates 11 centers across the Seward Peninsula and Saint Lawrence Island.3 Their Head Start programs are the only early education options in the region, serving about 240 Alaska Native children from remote villages and towns.4
Serving young children and families in remote areas requires creativity, as it comes with serious challenges.5 Supplies, food, and sometimes even staff must be flown out to these isolated communities weekly, which drives up costs. Accordingly, remote rural Alaskans are accustomed to paying more for necessities—even more than other Alaskans pay. Fuel must be shipped in on barges once each year; a gallon of milk can cost as much as 10 dollars; and village water systems can sometimes freeze up in the winter, forcing an entire town to use bottled water.6
Nevertheless, Kawerak Head Start has been able to make it work. Most of the region’s towns lack health service providers, so the program flies in a dentist, audiologist, and vision screener twice a year. But what may be typical expenses for the average Head Start program can be major expenses for Kawerak Head Start. Regular teacher trainings require flights to Anchorage, Alaska, which can cost $800 in addition to hotel and per diem costs. The harsh weather also takes its toll on program facilities and leaves some of Kawerak’s buildings in dire need of repair.7
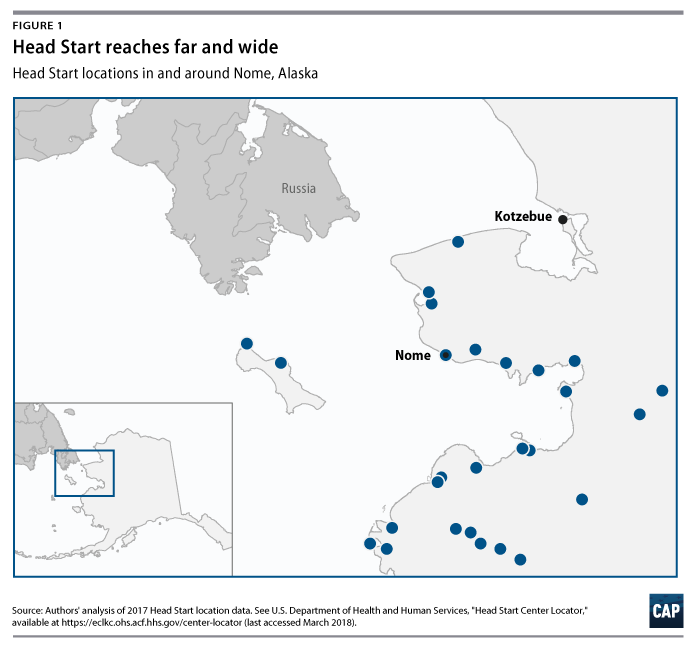
While Kawerak Head Start is an extreme example, its budgetary challenges and community needs resemble those of many other rural Head Start programs. It also embodies the mission of Head Start: to provide comprehensive services to young children and their parents no matter the challenges that might entail. Across the country, Head Start provides early education and medical, dental, and family services in areas where few other providers exist, bringing necessary resources to families where they live and work.
The very parts of country life that many rural residents cherish most—the undisturbed wilderness, the vast open spaces, and the independent lifestyle—can present enormous challenges when it comes to early education and service delivery. Low population density means that local governments and nonprofits face funding challenges and service delivery may become very costly when great distances are involved. As a result, resources and public services in rural areas tend to be scarce.8
At the same time, child poverty has been persistently high in rural areas.9 Due to rural communities’ physical isolation, it is usually more difficult to deliver services such as education, nutrition, and health care to families struggling to make ends meet.
For more than 50 years, Head Start has delivered a broad set of services to these struggling communities. Head Start helps vulnerable children by providing a comprehensive array of educational, nutritional, dental, medical, and mental health services. The programs also foster parental engagement, offer parent trainings and workshops, and connect families with a variety of social services that counter the innumerable daily challenges of living without consistent access to basic necessities.
In recent years, the benefits of Head Start have become even more clearly defined. Children who participate in Head Start have improved social-emotional and cognitive development; show higher levels of school readiness; and are more likely to graduate from high school and attend college.10 Head Start has even demonstrated intergenerational benefits, with reductions in teen parenthood and criminal behavior and increases in high school graduation and college enrollment rates for the children of Head Start alumni.11
Despite sometimes facing significant challenges, Head Start provides evidence-based, locally administered services to hundreds of thousands of rural children each year at one of the most critical stages of their development. This report assesses the scale and scope of Head Start in rural communities by analyzing Program Information Reports (PIR) from several thousand rural Head Start locations across the United States using geographic analysis tools to separate rural providers from their metropolitan counterparts as well as collecting insights via interviews with 20 rural Head Start administrators. For the purposes of this report, the authors use the general term “Head Start” to refer to the Early Head Start, Head Start, Migrant and Seasonal Head Start, and American Indian and Alaska Native Head Start programs. This report excludes Head Start locations in Puerto Rico and U.S. territories. (see Appendix for full methodological details)
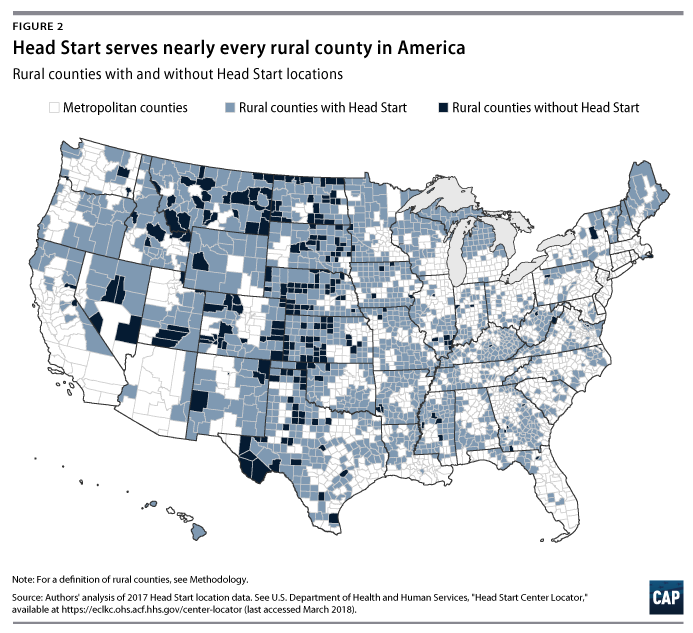
This comprehensive assessment finds that without Head Start, many rural counties would be left without any child care centers.12 Head Start currently operates programs in nearly every rural county in the United States and is often the sole service provider for families in remote communities suffering from persistent, deep poverty.13
Key findings from this report include:
- Head Start has centers in 86 percent of America’s 1,760 rural counties. (see Figure 2)
- In the 2015-2016 program year, rural Head Start programs enrolled more than 175,000 children, employed nearly 50,000 staff, and delivered family services to more than 110,000 families.
- Within a 10-state sample, this study finds that 1 out of every 3 rural child care centers is a Head Start program.
- Across those 10 states, CAP identifies 48 counties that would have no child care centers if not for Head Start.
- Despite higher poverty rates, fewer resources, and unique challenges, rural Head Start programs provide children with an evidence-based early education and connect families with critical services at rates similar to those of Head Start programs in metropolitan areas.
Rural Head Start programs help fill a crucial role in delivering educational, health, and parent education services to families with few other options for assistance. Furthermore, these programs are often the only high-quality early education programs in rural communities, which helps parents work the hours necessary to get back on their feet.
Background
The United States is the wealthiest nation on earth, yet it ranks near the bottom of the world’s advanced economies in terms of child poverty—above only a few, significantly poorer countries.14 According to recent estimates, more than 1 in 5 children in the United States lived in households below the federal poverty line.15 American children currently comprise 23 percent of the overall population but represent 33 percent of those living in poverty.16
The nation’s youngest children—those under age 6—are more likely to experience poverty than any other age group.17 American families with young children have significantly lower incomes than similar households without children, or those in which children have reached school age.18 In the absence of policies that help cover the costs of parental leave, child care, or the everyday expenses that children bring, young parents are often strained by low wages, irregular hours, and household debt.19
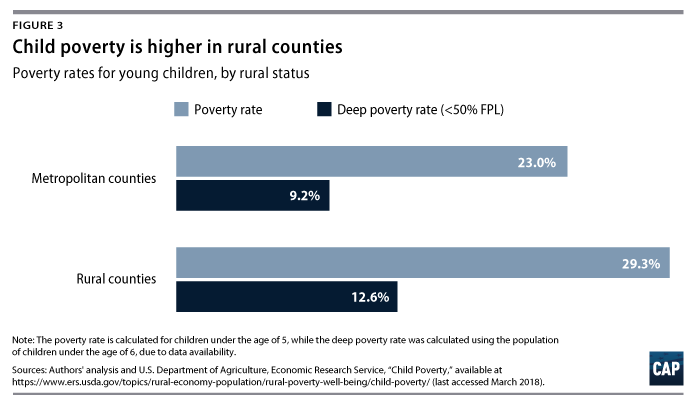
These hardships are particularly acute for rural families, resulting in child poverty being significantly worse in rural areas than in metropolitan areas. By the definition of rural used in this report (see text box below), more than 29 percent of rural children under age 5 live in poverty, compared with 23 percent of young children in metropolitan counties.20 (see Figure 3) Children living in rural areas are also more likely to experience deep poverty, which for a family of four means living on an income of less than $1,000 per month.21 This study finds that young children in rural counties are 37 percent more likely to live in deep poverty than their metropolitan peers.22
Head Start plays a critical role in mitigating the effects of poverty for children and families in rural areas. The experience of poverty can cause toxic stress, meaning that both children and their families need added supports.23 In low-density rural areas, however, these resources may be hard to find or many miles away. Head Start has been designed to be geographically dispersed and to connect families with a variety of wraparound services in addition to high-quality early education.24
What does “rural” mean, anyway?
Research on rural communities can be complicated since there are several competing definitions of “rural.” According to the U.S. Census Bureau, any small town with more than 2,500 residents is coded as an urban cluster, even though many of these small-town residents would consider themselves rural dwellers. For this report, therefore, the authors use the rural-urban continuum codes developed by the U.S. Department of Agriculture’s Economic Research Service (USDA-ERS). These codes place each American county into 1 of 9 categories, with 1 being the most urban and 9 being the most rural.25 This report defines any county between 5 and 9 on this spectrum as rural, which produces 1,790 rural counties.
To aid in the study of rural economic characteristics, USDA-ERS developed county-level designations to track county conditions such as population loss, low employment, and persistent child poverty. Looking closer at the counties designated as persistent child poverty counties—in which the child poverty rate has been greater than 20 percent since 1980—this study finds that 75 percent are rural.26 Head Start serves 95 percent of these USDA-designated persistent child poverty counties, funding annual enrollment of nearly 75,000 children across more than 4,000 classrooms.27
Although Head Start plays an important role in helping rural families, there is a dearth of research on how Head Start programs in rural areas serve families when compared with overall Head Start service rates. The limited research on rural early education shows that children in rural America are less likely to attend early childhood education programs. One study found that 34 percent of children in the most rural census tracts entered kindergarten without any prior preschool participation, compared with only 24 percent in nonrural areas.28 Another major study noted that “research on Head Start and related educational programs for low-income children has historically focused almost exclusively on low-income, urban environments.”29
This report explores the critical role that Head Start plays in rural areas using findings from analyses of data from the 2015-16 Head Start Program Information Report and interviews with rural Head Start administrators. (see Appendix)
Key findings
This section outlines findings from an original analysis of Head Start in rural areas. The section first presents data on the number of children enrolled and staff employed in rural Head Start programs. It then highlights the important role that Head Start fills in the supply of center-based child care in rural child care deserts. Finally, it presents findings on the scale and scope of comprehensive health and family services delivered to rural families through Head Start and compares service delivery rates among rural and metropolitan programs.
Enrollment and staffing
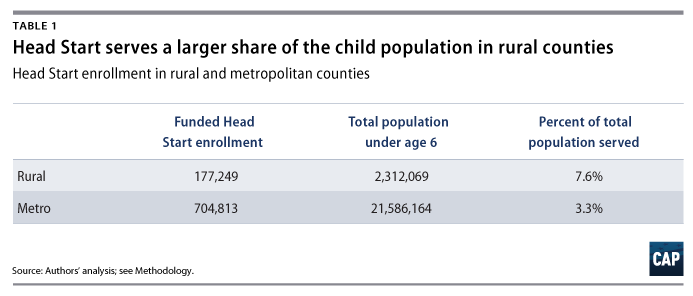
In the 2015-2016 program year there were 177,249 federally funded Head Start slots across 10,165 classrooms in rural counties. This accounts for about one-fifth of total Head Start enrollment in the United States. (see Table A2 in the Appendix for Head Start enrollment by state and rural status) Compared with metropolitan areas, in rural areas, Head Start serves a larger share of the population of children under age 6.
Head Start employs nearly 50,000 staff in rural areas. Well over a quarter—29 percent—of staff in rural Head Start classrooms are current or former parents. This is significantly greater than the just one-fifth—20 percent—of staff in metropolitan area classrooms.
Head Start in rural child care deserts
“If not for Head Start, there would be a lot of families that wouldn’t be able to get training, go to school, or look for jobs because there’s nowhere for their kids to stay.”
–Mississippi Head Start advocate30
In a prior 22-state investigation of licensed child care supply, CAP found that small towns and rural areas with below-average median family incomes faced the deepest shortage of child care. These areas, referred to in the research as child care deserts, are home to approximately 3 in 5 rural Americans.31 These findings prompted the question of whether Head Start is potentially working to fill a gap in available quality child care for these undersupplied communities.
Many rural families living below the federal poverty line are working families. Fifty-five percent of rural Head Start children have at least one employed parent.32 (see Table A4) Interviews with rural Head Start administrators repeatedly confirmed that while most Head Start parents are working, many are working low-wage jobs, often with nontraditional or inconsistent hours.33 As one Kansas director explained, “Quality child care is difficult for our families to find. Most families work; they work low-paying jobs, often not full time. [This is a] major challenge for families.”34
These findings align with much of the research literature, which finds that rural families have unique child care needs.35 Often there are very few quality child care options within a reasonable distance, and parents resort to using unlicensed care that is not regularly inspected.36 While Head Start provides localized services that match community needs, the program boasts evidence-based quality standards that must be implemented regardless of location.37 According to one Missouri Head Start director, “there are two counties [in the region] where there is no licensed child care. Even when they are operating legally, the standards are not up to the Head Start quality.”38
For families living paycheck to paycheck, any quality child care options would likely be unaffordable, even with state child care subsidies, which usually only cover a portion of the child care bill.39 Finding qualified teachers and staff also poses a significant challenge for rural programs and could contribute to the dearth of child care in rural areas.
Head Start programs represent approximately one-third of the center-based child care supply in these states’ rural counties.
CAP’s analysis of a 10-state sample reveals that Head Start programs represent approximately one-third of the center-based child care supply in these states’ rural counties. In terms of child care slots, rural Head Start programs in these 10 states represent 22 percent of the overall child care capacity, even when including home-based care. To conduct this portion of the analysis, this study examined 739 rural counties across 10 states, comprising 40 percent of the rural population of the United States. These 10 states have the highest number of rural counties among the states with publicly available data on child care locations. (see Methodology)
Since Head Start mostly serves 3- and 4-year-olds, the authors compared Head Start supply to center-based child care supply. This is because a majority of parents prefer center-based care for their 3- and 4-year-olds.40 Among the 739 rural counties studied, there were nearly 1,900 Head Start centers, while there were around 4,000 other child care centers.
The study also finds that, when excluding Head Start, one-quarter of the rural counties in the 10-state sample have either zero or only one child care center. These underserved rural counties would have almost no child care centers available to families were it not for Head Start. In fact, across these undersupplied rural counties, Head Start accounts for more than 70 percent of the center-based child care supply—252 Head Start providers versus 103 non-Head Start child care centers.
Head Start fills an especially large gap in very remote rural counties, sometimes referred to as “frontier counties.”41 Using USDA-ERS rural-urban codes 8 and 9 to identify frontier counties, the authors analyzed the supply of licensed center-based care versus Head Start locations. Among the frontier counties contained in this 10-state sample, Head Start programs represent nearly half of the center-based child care supply.42 (see Figure 4)
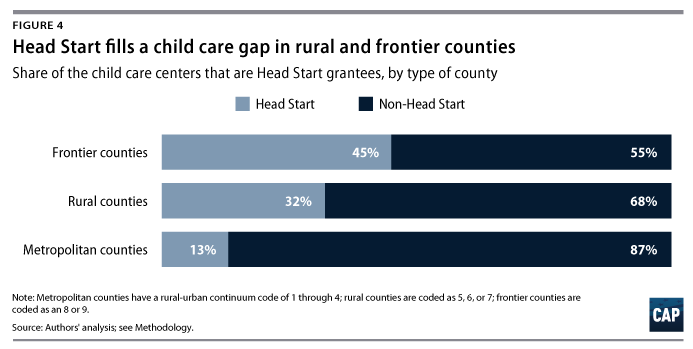
This analysis identifies 48 counties in the sample in which Head Start was the only center-based child care provider.43 These counties, which are spread across 9 of the 10 states in the sample, can be found in the Appendix. It is not hyperbole to say that without Head Start, there would be no child care centers to educate and care for young children in these counties.
All Head Start providers must meet high-quality federal standards that encompass children’s cognitive, socio-emotional, and physical development, which means that in areas with few other child care options, Head Start is often the highest-quality preschool in rural areas.44 This assessment is backed up by the fact that the Head Start Impact Study report—the gold-standard evaluation of the program—found that Head Start’s largest and longest-lasting positive effects were concentrated among rural providers. The 2010 study found that 3-year-olds who attend Head Start programs in rural areas experienced significant and longer-lasting cognitive benefits and greater socio-emotional development than their urban peers.45 It is possible that Head Start had this outsized impact in rural areas due to shortages of high-quality alternatives to rural Head Start, whereas metropolitan areas feature a greater number of high-quality alternatives. The results of this analysis align with that hypothesis.
Comprehensive services
“One of the things that is important about Head Start is the family approach. If there are issues that are keeping that family from reaching their full potential, Head Start connects people with the local and sometimes state resources to improve their situation.”
–Mississippi Head Start advocate46
Head Start is a two-generation program, meaning that it targets services to both low-income children and their parents to promote family wellbeing. Particularly for families in underserved rural areas, Head Start may be the first point of contact with trained service providers who can make referrals to community resources.
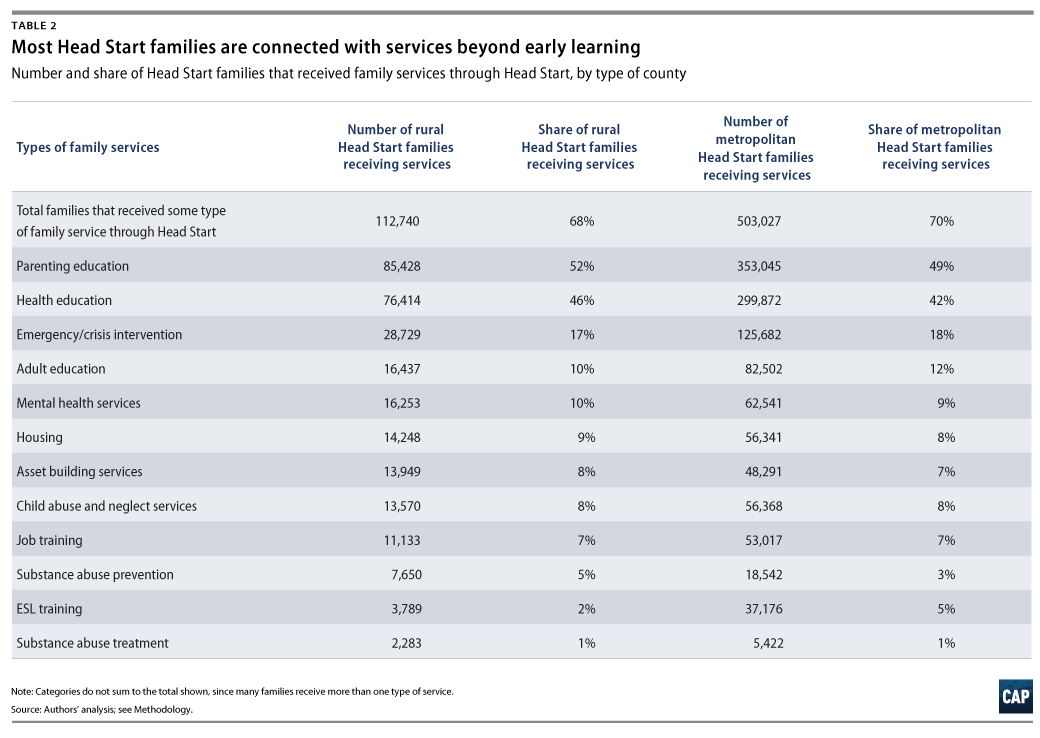
In the 2015-2016 program year, 68 percent of rural Head Start families received some type of family service through Head Start. (see Table 2) This includes services such as parenting education, job training, and substance abuse prevention.
Health services
“In a lot of cases, Head Start is the only program in town. Often a pediatrician will say, you need to take your kids to Head Start or Early Head Start so that they can get help for these developmental delays.”
–Mississippi Head Start advocate47
In many rural areas, Head Start is one of the only health care providers and connects children to services they may not otherwise receive. The U.S. Health Resource and Services Administration designates Health Professional Shortage Areas (HPSAs) based on the availability of primary care, dental, and mental health providers in the nearby area.48 CAP’s analysis finds that the overwhelming majority of HPSAs are located in rural counties.49 Not surprisingly, children in rural areas receive fewer health care services than children in metropolitan areas. According to the 2011-2012 National Survey of Children’s Health, children in rural areas were less likely to have had a preventive health or dental care visit in the past 12 months than were children in metropolitan areas.50
Head Start is present in about 80 percent of rural HPSA counties and provides thousands of rural children with the necessary health and developmental screening services they need to thrive.51 Despite deep shortages in dental and mental health professionals in rural areas, Head Start programs connect families with dental and mental health services at rates comparable to areas with greater service coverage.
Rural children typically enter Head Start having had lower rates of access to important services than children in metropolitan areas. (see Figure 5) The analysis shows, for example, that 90 percent of metropolitan Head Start children are up-to-date on their immunizations at the beginning of the school year, compared with just 83 percent of rural Head Start children. These gaps persist, as children in rural Head Start programs remain behind their metropolitan peers in rates of service receipt through the end of the year.
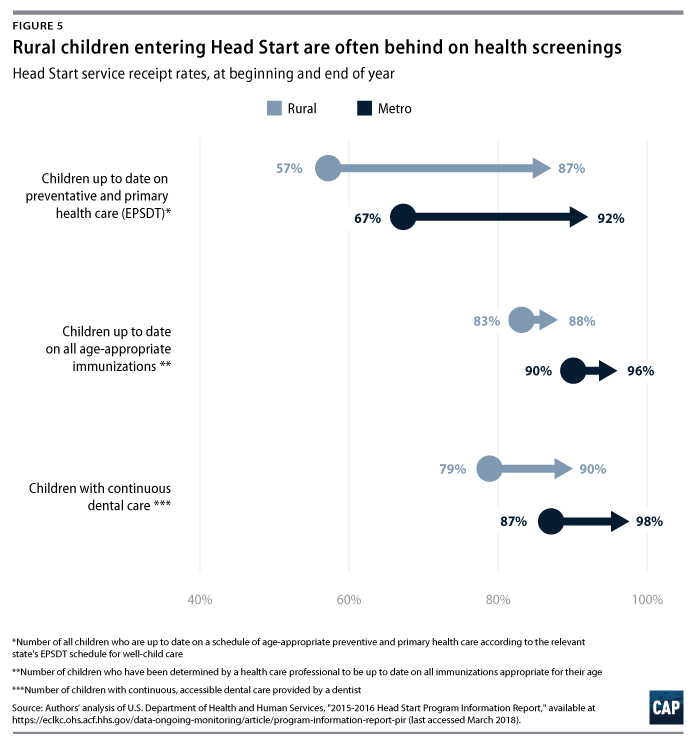
However, rural Head Start programs are bringing children up-to-date on screenings and immunizations at similar rates to programs in metropolitan areas. Despite the fact that rural children are starting behind, Head Start makes similar progress in connecting children with services. End-of-year rates of Early and Periodic Screening, Diagnostic, and Training, immunizations, and dental service receipt are lower for children in rural areas, yet they still increased by roughly the same amount as rates for metropolitan children over the course of the 2015-2016 school year. Even Head Start programs in areas designated as HPSAs seem to successfully overcome challenges to provide health services to young children: Interestingly, Head Start providers in rural primary care HPSAs vaccinate a higher percentage of their children than rural non-HPSAs—12 percent versus 8 percent. This may be because rural children living in HPSAs often miss their vaccinations due to primary care shortages.
Head Start and the rural drug overdose epidemic
“There is lots of substance abuse across the service area, lots of family trauma and mental health—these things are exacerbated in a rural community because there are no resources to help with those. Families have so many stressors in their lives but are unable to get connected with the services to alleviate stressors. There’s nowhere to go for help.”
–Montana Head Start director52
In October 2017, the Centers for Disease Control and Prevention (CDC) issued a press release announcing that drug overdose deaths have been steadily rising in rural areas and have now surpassed the overdose death rates in metropolitan areas.53 This has largely been driven by massive increases in illicit prescription and opioid drug use. In the past 15 years, the opioid death rate has quadrupled among young adults in rural areas.54
Head Start programs are on the front line of the opioid epidemic and are uniquely positioned to take a full family approach to addressing the deep and damaging effects of drug addiction. Programs work to prevent harm and promote healthy child development for Head Start children, while connecting parents and families with the services they need to address drug misuse and cope with the accompanying trauma. Head Start offers relevant services to families, including substance abuse prevention and treatment services, child abuse and neglect services, parent coaching, domestic violence services, and more. (see Table 2
In the course of this research, the authors analyzed CDC drug overdose death rates from 2011-2015, the most recent years for which data are available. CAP’s study found that, of the 100 counties with drug overdose death rates more than twice the national average—known as drug epidemic counties—63 counties were rural.55 Examining program data from rural Head Start providers in these areas reveals several important findings about the role of Head Start in these rural drug epidemic counties.56
Consider some snapshots of the rural drug epidemic from the Head Start Program Information Report:
- Head Start enrolls more than 10,000 children in these 63 rural drug epidemic counties.
- In rural counties, Head Start families both reported a greater need for substance abuse prevention and treatment services and received these services at a higher rate than families in metropolitan counties.
- In rural drug epidemic counties, 16 percent of Head Start families received child abuse and neglect services, compared with only 8 percent of families in all other rural counties.
- In rural drug epidemic counties, Head Start families receive domestic violence services at more than twice the rate of other rural counties—6 percent versus 2.5 percent.
- In rural drug epidemic counties, 5 percent of children in Head Start lives with their grandparent(s), compared with 3 percent of children in other rural counties and only 2 percent of children in metropolitan counties.
Lessons from the ground
As this report shows, many rural Head Start programs are filling important gaps in early education and service delivery despite limited resources, a lack of rural service providers, and other barriers. This section explores the innovative ways that rural Head Start programs have been able to navigate these challenges and highlights three key themes that emerged from interviews with 20 state Head Start leaders in Alaska, Kansas, Mississippi, Missouri, Montana, and Nebraska. Given the small sample size, the authors encourage further exploration and research on these topics.
Staffing in rural areas: “We have to grow our own here”
Employing qualified and committed teachers is paramount to running a successful early childhood program. Acting as a model for quality early childhood education, Head Start has adopted certain standards for teacher education and training. The 2007 Head Start Act, for example, mandated that at least half of Head Start teachers have a bachelor’s degree in early childhood or a related field by 2013, and in 2016, about three-quarters of teachers held a bachelor’s degree.57 Despite these increased credential requirements, wages for Head Start teachers remain low: In 2016, the average Head Start teacher earned just $32,000.58
State interviewees overwhelmingly identified finding and retaining qualified staff as an area that requires unique approaches in their communities. In rural areas, there is a limited pool of qualified applicants for teaching positions: Compared with 20 percent of adults in metropolitan areas, only 12 percent of rural Americans hold a bachelor’s degree, and the pool of applicants with a degree in early education is even more limited.59 Professional development for current teachers can be very expensive for rural programs, as paying for long distance travel, training fees, and lost wages is more than rural programs can typically afford.60
As is common in the field of early childhood education, once teachers have attained higher credentials, they often leave for more competitive salaries teaching preschool or kindergarten in the local school system.61 And just as in early education programs across the country, high rates of teacher turnover leave many rural programs in a constant search for qualified staff. One Montana regional director said their program had not had a steady teacher in place for two years, while a director in Missouri noticed that constantly recruiting new teachers had compromised their program quality and negatively affected children.62
Rural interviewees identified growing their own—training and employing current and former Head Start parents—as an effective strategy for retaining committed staff. A state advocate from Nebraska explained that training parents to work as classroom aides, teaching assistants, or lead teachers is worth the investment because “they’re loyal, they believe in the program, and they’re great with other families. That’s how we get people that stick around.”63
This analysis confirms this innovative strategy, finding that rural Head Start programs employ a significantly higher percentage of parent staff than metropolitan programs: 29 percent of staff in rural Head Start programs are current or former parents, compared with 22 percent in metropolitan areas.64
Transportation: “Without transportation, you don’t have a program”
A dispersed population can be an insurmountable barrier for other service providers to operate in rural and frontier areas. Head Start providers must work to overcome the challenge of getting to and from Head Start centers. This can be especially challenging for low-income parents who might not have consistent access to a reliable vehicle or who may not have the time or money to bring children of different ages to multiple locations for preschool and school drop-offs.
Head Start interviewees reported that providing transportation is essential to keeping the programs fully enrolled and that without it, they see drops in attendance. As one Montana director explained, “If we stopped providing transportation, we would end up with an under-enrollment issue. On days in the winter when you can’t run the bus, our program’s attendance drops by 50 percent.”65 Inconsistent attendance can have significant consequences for a child’s learning and development, as it disrupts their routine and can undermine the progress that they have made in Head Start.66
Head Start does not require grantees to provide transportation services, but transportation is essential for most rural programs. The costs of providing transportation add up quickly. In addition to renting or purchasing buses that are equipped with integrated seating designed to safely carry young children, programs must pay for gas, insurance, and personnel. Head Start programs must hire multiple staff members who are trained as drivers and bus monitors—positions that are difficult to fill due to the low pay and unusual hours. In frontier areas, especially, buses cover vast distances, which is time-consuming and even more expensive. The Montana director estimates that their program’s bus travels about 220 miles each day.67
Some programs have partnered with local school districts or utilized public transit routes to help transport children to Head Start centers and save a significant amount of money. Several programs’ transportation arrangements have been integrated into the local school systems’ bus routes, particularly in programs that are housed in local elementary schools. Other programs have worked with local schools to establish a single drop-off point—so that families can bring multiple children to one location—in an effort to boost consistent attendance.
Partnerships with the local community: “People tend to know each other out here”
Head Start programs in rural areas leverage relationships within their local communities to ensure that children and families receive the services they need. Nearly all interviewees emphasized that these partnerships are vital to their programs’ ability to deliver services in the face of the extensive challenges of living in a rural area. As one Head Start director said, “People tend to know each other out here, and those working relationships are why we are still able to exist.”68
Interviewees highlighted local community colleges as valuable partners both for providing needed services to children and for developing credentialed Head Start teachers. One program in Nebraska partners with local community college dentistry students who provide free dental checkups to Head Start children.69 Without the community college, this program would have difficulty providing dental services due to the dearth of pediatric dentists in the area. Community colleges with programs in early childhood education also help bolster the supply of new Head Start teachers, as well as provide professional development and educational opportunities for current Head Start teachers.
Head Start is also a valuable partner in rural areas, as the benefits of the program often extend to non-Head Start children in the community. Head Start funds cannot support children who are not enrolled in the program, but some resources or equipment may benefit the broader community. When Head Start partners with service providers for enrolled children, for example, some of those providers will also offer services to non-Head Start children in the classroom, school, or community at large. This makes important services such as vaccinations, hearing and vision screenings, lead screenings, and dental check-ups available to non-Head Start rural children who may not otherwise have access to them.
As a Head Start director in Nebraska explained, “We offer Head Start services to everyone that comes to the preschool, which extends services beyond Head Start kids … We do the health fair and everyone benefits.”70 A director in Kansas took a similar approach with rural dental clinics, noting, “We’ve bought mobile dental equipment and go to each of our sites three times per year. We partner with several people. We’ll loan out our equipment for them to use it at the school because providing dental is very hard.”71 They explain that once the medical personnel and equipment are paid for and available, serving additional children comes at no additional cost to Head Start. This spillover into the local community means that the number of children receiving medical services through Head Start in rural areas is likely an underestimation.
Conclusion
For too long, policymakers in Washington have unilaterally focused on the academic outcomes of children who attend Head Start. The findings in this report suggest that such a one-dimensional policy debate ignores the fact that without Head Start, many rural children would lack access to the quality early education and health services that are critical to their development. Head Start meets families where they are—economically, geographically, and emotionally—and brings services to the most remote parts of the United States. The rural American children and families who participate in Head Start would be better served if policymakers focused on opportunities to bolster resources and support for providers in order to address communities’ unique challenges and budgetary constraints.
About the authors
Rasheed A. Malik is a senior policy analyst for Early Childhood Policy at American Progress. His work focuses on child care infrastructure and supply, the economic benefits of child care, and bias and discrimination in early childhood policy. Malik’s research has been cited by NPR, HLN, The Washington Post, Slate, CNNMoney, The Guardian, and Newsweek, among others.
Leila Schochet is the research and advocacy manager for Early Childhood Policy at American Progress. Prior to joining American Progress, Schochet conducted senior research around staff retention and wellness in child care centers in Addison County, Vermont. She also interned at the Institute for Educational Leadership, where her work focused on communicating the importance of family and community engagement in education.
Acknowledgments
The authors would like to thank their colleagues at the Center for American Progress for their helpful insights and careful review of this report: CJ Libassi, Heidi Schultheis, Andrew Schwartz, Katie Hamm, and the Art and Editorial team. The authors would like to acknowledge the National Head Start Association for their help connecting the authors with its state affiliates and verifying information in this report. Finally, the authors wish to thank the 20 rural Head Start interviewees for taking the time to share their experiences and for the important work they do each day.